As a licensed mental health provider professional, mastering the intricacies of CPT codes is crucial for accurate medical billing and optimal reimbursement.
This comprehensive guide for healthcare professionals focuses on CPT code 90791, one of the most important codes for initial psychiatric diagnostic interview evaluations. We'll cover everything from basic definitions to reimbursement rates and the use of add-on codes for extended sessions.
For a comprehensive guide to all CPT codes with cheat sheet and examples, refer here.
What is CPT Code 90791?
CPT code 90791 stands for "Psychiatric diagnostic evaluation." It is used to bill for a comprehensive initial assessment of the mental health condition a new patient (initial appointment session) or an established patient presenting with a new behavioral health concerns. This code covers an integrated biopsychosocial assessment, including:
- Patient history
- Mental status examination
- Diagnostic evaluation
- Treatment recommendations
It's important to note that 90791 does NOT include any medical services or procedures, such as prescribing medication.
For any new patient, the first intake session is usually billed as 90791, with subsequent sessions billed as 90834 or 90837, depending on the duration of session.
How long is a session for 90791?
While CPT code 90791 is not time-specific, the typical duration for this type of evaluation is between 45 to 60 minutes. However, the Centers for Medicare & Medicaid Services (CMS) states that the minimum time for billing 90791 is 16 minutes, with a maximum of 90 minutes before requiring additional coding.
Many practitioners find that a thorough initial evaluation often takes closer to 60 minutes or more to complete all necessary components. For sessions extending beyond 90 minutes, you'll need to use add-on codes, which we'll discuss in the next section.
Who Can Bill CPT Code 90791?
The following licensed behavioral health providers and mental health professionals providing psychotherapy services can typically bill using CPT code 90791:
- Licensed Clinical Social Workers (LCSW)
- Licensed Professional Counselors (LPC)
- Licensed Mental Health Counselors (LMHC)
- Licensed Marriage and Family Therapists (LMFT)
- Clinical Psychologists
- Psychiatrists
Always check with your state regulations and insurance providers for specific requirements, as they may vary.
Does 90791 Require Authorization?
In most cases, CPT code 90791 is considered a routine outpatient service and does not require prior authorization. However, it's important to note that policies can vary between insurance providers and specific plans. Some key points to consider:
- Some insurance companies may require authorization for all mental health services, including initial evaluations.
- Certain plans might have limits on the number of mental health visits allowed without authorization.
- For some providers, like United Healthcare, you might need to ensure that 90791 is specifically included in the authorization if one is required.
Best practice is to verify benefits and authorization requirements for each client before their initial appointment. This can help prevent claim denials and ensure smooth reimbursement.
Does 90791 Pay More Than a Normal Session?
Yes, typically CPT code 90791 is reimbursed at a higher rate than standard therapy sessions. Here's what you need to know for your initial intake appointment billing:
- Reimbursement for 90791 is generally 35-75% higher than that of a standard 45-minute therapy session (90834).
- It can be 10-50% higher than the reimbursement for a 60-minute therapy session (90837).
- The exact difference in reimbursement varies depending on factors such as:
- Your credentials
- Geographic location
- Specific insurance plan
- Contracted rates
The higher reimbursement rate reflects the comprehensive nature of the initial evaluation and the additional time and expertise required to complete it thoroughly.
Typical Reimbursement Rates for 90791
Understanding the typical reimbursement rates for CPT code 90791 can help you better manage your practice's finances and set appropriate expectations. It's important to note that these rates can vary significantly based on factors such as geographic location, provider type, and specific insurance plans. Here's an overview of typical reimbursement rates:
Medicare Reimbursement Rates
Medicare rates for medicare services often serve as a baseline for other insurance providers. According to the Centers for Medicare & Medicaid Services (CMS), the national average reimbursement rates for CPT code 90791 in recent years were:
- 2024: $172.10
- 2023: $174.86
- 2022: $195.46
- 2021: $180.75
- 2020: $145.44
Private Insurance Reimbursement Rates
Private insurance reimbursement rates can vary widely but often fall within the following ranges:
- For Masters-level providers (e.g., LCSWs, LPCs): $90 - $150
- For Doctoral-level providers (e.g., Psychologists): $110 - $200
- For Psychiatrists: $150 - $300
Using Add-On Codes with 90791
For initial evaluations that extend beyond 90 minutes, you can use add-on CPT codes to accurately bill for the additional time spent. The primary add-on CPT codes used with 90791 are:
- +99354: Prolonged evaluation and management service, first hour
Use this code for sessions lasting between 91-150 minutes (90791 + first hour of extended time) - +99355: Prolonged evaluation and management service, each additional 30 minutes
Use this code in conjunction with 99354 for sessions extending beyond 150 minutes
Here's how to apply these codes:
- 90-minute session: Bill only 90791
- 91-150 minute session: Bill 90791 + 99354
- 151-180 minute session: Bill 90791 + 99354 + 99355
- 181-210 minute session: Bill 90791 + 99354 + 99355 x 2
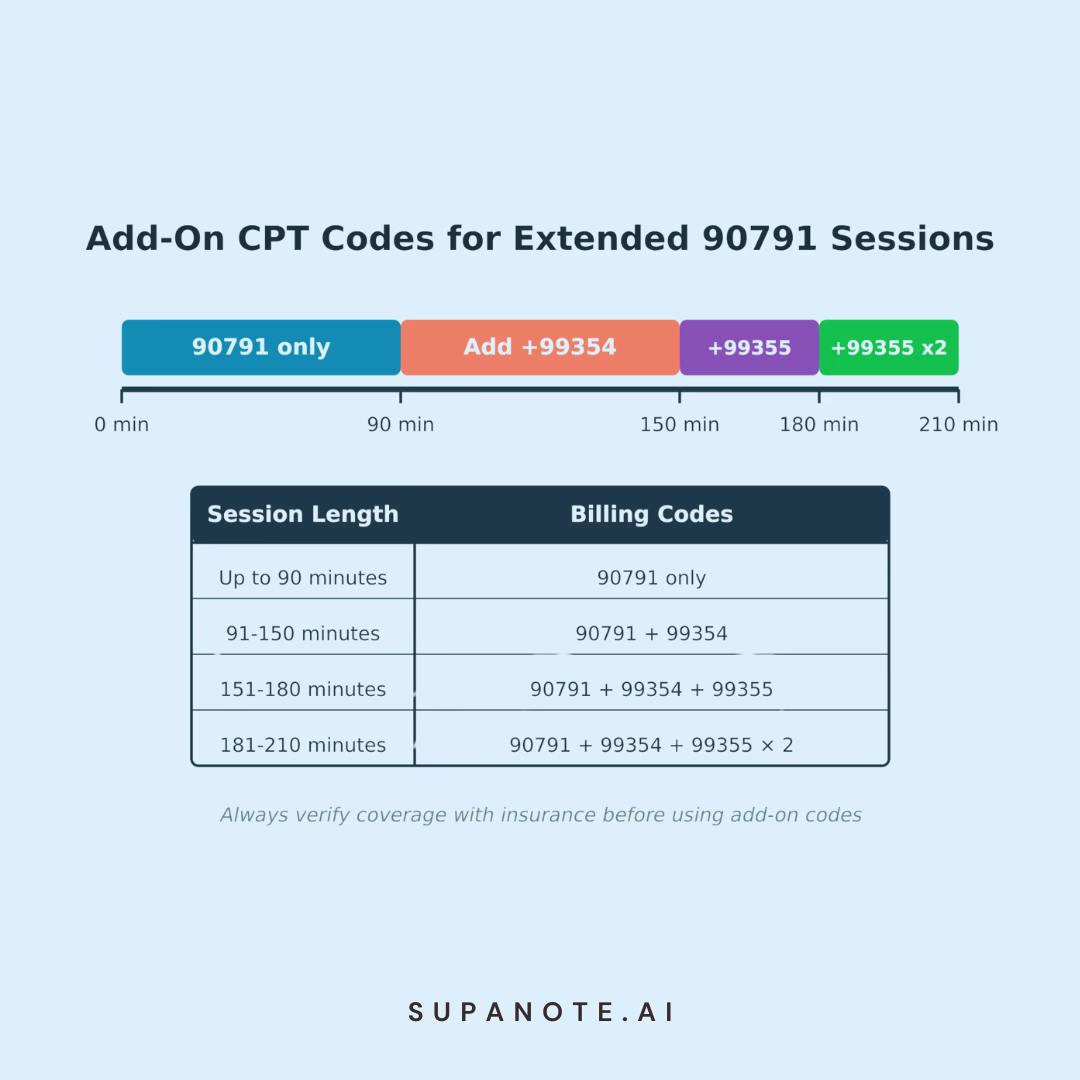
Remember, not all insurance plans cover these add-on codes, so it's crucial to verify coverage before using them. Also, ensure your documentation clearly justifies the need for extended session time.
Frequency of Billing
The frequency of billing CPT code 90791 is generally limited. Most insurance providers allow this code to be billed only once per year, per client, per provider. However, some plans may allow it to be billed once every six months.
It's crucial to verify the specific rules with each insurance provider, as policies can vary. If you need to perform another comprehensive evaluation within the same year, you may need to use a different code or obtain special authorization.
CPT Code 90791 vs. 90792
According to the cpt manual, it's important to understand the difference between CPT codes 90791 and 90792 when considering a medical evaluation:
- 90791: Psychiatric diagnostic evaluation without medical services
- 90792: Psychiatric diagnostic evaluation with medical services
The key difference is that 90792 includes medical services, such as prescribing medication or ordering laboratory tests. This code can only be used by providers who can perform these medical services, typically psychiatrists or psychiatric nurse practitioners.
Common Pitfalls and Best Practices
To ensure proper use of CPT code 90791, keep these best practices in mind:
- Don't use 90791 for every session with a client. It's specifically for initial evaluations or reassessments of new problems.
- Ensure your documentation thoroughly supports the use of this code and any add-on codes. Make sure to mention mental status and accurate diagnosis
- Be aware of frequency limitations set by insurance providers.
- Don't use 90791 and psychotherapy codes (like 90834 or 90837) on the same day for the same client.
- When using add-on codes, make sure they're covered by the client's insurance plan.
- Regularly audit your billing practices to ensure compliance.
- Stay updated on any changes to coding guidelines or reimbursement policies.
Documentation Requirements
Proper documentation is crucial when billing CPT code 90791. For licensed clinical social workers and other providers, your clinical notes should include a complete medical assessment with:
- Chief complaint and history of present illness
- Relevant psychiatric history
- Relevant medical history
- Substance use history
- Family psychiatric and medical history
- Psychosocial history
- Mental status examination
- Risk assessment
- Diagnostic evaluation
- Treatment recommendations and plan
If you're using add-on codes, be sure to document:
- Start and end times of the session
- Justification for the extended session time
- Additional assessments or interventions performed during the extended time
Ensure your documentation clearly supports the need for a comprehensive evaluation and justifies the use of CPT code 90791 and any add-on codes.
Refer to our detailed guides on writing case conceptualization, biosychosocial and psychosocial assessments.
Automate your documentation with AI Therapy Note tools
Documentation is probably the least favorite activity of any mental health professional.
Did you know that now AI tools can write your Intake notes?
Technology has progressed such that there are now several AI products purpose-built for mental health professionals, that can listen in to your sessions and automatically generate robust, insurance-compliant Intake Notes. They can even write give suggestions for mental health assessment and possible mental health diagnosis.
Supanote is the leading AI Therapy Note tool - Supanote comes with prebuilt intake form templates and can accurately capture your intake session into an insurance-compliant note for billing with 90791. Curious? Here's a detailed guide to AI Therapy Note tools and how they work.
Get your Personal AI Scribe
Let Supanote handle the 90791 documentation burden while you focus on what matters most - your patients
Try Supanote for Free Now!
Frequently Asked Questions
Q. How often can I bill 90791 for a single client?
A. Typically, once per year per provider. Some insurance plans may allow it every six months. Always verify with the specific insurance provider.
Q. What's the difference between 90791 and 90792?
A. 90791 is for psychiatric evaluations without medical services, while 90792 includes medical services and can only be used by providers who can prescribe medication.
Q. How long should a 90791 session be?
A. While there's no set time, these sessions typically last 45-60 minutes. As per CMS, the minimum is 16 minutes, and the maximum is 90 minutes before additional coding is required.
Q. Can I bill 90791 for an existing client with a new problem?
A. Yes, if a comprehensive reassessment is necessary due to a new problem or significant changes in the client's condition.
Q. What if my evaluation takes longer than 90 minutes?
A. You can use add-on codes like +99354 and +99355 for extended sessions. Always check with the insurance provider for their specific policies on these codes.
Q. Can I use 90791 for couples or family therapy initial evaluations?
A. While 90791 is typically used for individual evaluations, some providers use it for initial couple or family sessions. However, it's best to check with the specific insurance provider for their policy on this usage.
Q. Are there any modifiers I should use with 90791?
A. In most cases, no modifiers are needed with 90791. However, if you're providing services via telehealth, you may need to use the appropriate telehealth modifier as required by the insurance provider.
Q. Can 90791 be billed telehealth?
A. Yes, CPT code 90791 can be billed for telehealth with appropriate telehealth modifiers (GT or 95) and the correct Place of Service code (typically POS 02). Always verify specific telehealth requirements with each insurance carrier, as coverage policies and documentation requirements may vary.
Conclusion
Mastering the use of CPT code 90791 is essential for licensed mental counselors and mental health practitioners to ensure proper medical billing and maintain compliance.This code allows for comprehensive initial evaluations, setting the foundation for effective treatment planning. By understanding the nuances of 90791, including session length limitations, documentation requirements, and the use of add-on codes, you can optimize your billing practices while focusing on providing high-quality care to your clients.
Remember to stay informed about any changes in coding practices or insurance policies, as the healthcare landscape is continually evolving. When in doubt, don't hesitate to consult with billing specialists or contact insurance providers directly for clarification.
By following the guidelines and best practices outlined in this guide, you'll be well-equipped to navigate the complexities of mental health billing, ensuring that clinical psychologists, licensed professional counselors, and licensed marriage family therapists are fairly compensated for the vital services you provide to your clients.
Ready to try? 10 notes on us!
Login to your Supanote account and instantly access 10 free notes
Try Supanote for Free Now!