AI SOAP notes are transforming how mental health professionals handle clinical documentation. These intelligent ai tools convert your therapy sessions into properly formatted SOAP note documentation automatically.
The result? You spend less time writing and more time with patient care. This comprehensive review covers 8 leading AI soap note generator tools, comparing their pricing, features, and suitability for different practice types.
You’ll discover which note generator options offer native EHR integration, mental health-specific note templates, and the best value for your practice size.
What Are AI SOAP Notes?
AI SOAP notes are digital clinical documentation tools that automatically convert your therapy sessions into structured, professional notes using AI. These AI generated soap notes streamline the documentation process for healthcare professionals.
SOAP Format Breakdown
The SOAP format follows four essential components:
- Subjective (client’s reported experience)
- Objective (observable behaviors)
- Assessment (clinical impressions)
- Plan (treatment interventions).
This structure is critical for mental health documentation because it ensures comprehensive record-keeping and meets legal and insurance requirements.
Traditional manual SOAP note writing presents significant challenges. You’re spending 15-30 minutes per patient visit writing notes, often staying late or taking work home.
The repetitive nature leads to documentation fatigue, and you risk missing important details or creating inconsistent formatting across cases. Healthcare professionals need standardized methods to document patient encounters efficiently.
How AI Transforms SOAP Note Creation
AI SOAP note tools record your sessions and automatically generate structured clinical notes. The technology analyzes speech patterns, identifies key therapeutic moments, and organizes relevant information into proper soap format.
You’ll encounter two main approaches: template-based systems that fit information into predefined structures, and free-form AI that adapts to your unique note taking style. The best soap note AI tools integrate directly with your existing EHR system, eliminating the copy-paste workflow that disrupts your clinical routine.
Why Mental Health Professionals are switching to AI SOAP Notes
The shift to AI soap notes isn’t just about keeping up with technology—it’s about reclaiming your practice and improving patient care. Healthcare providers are discovering significant benefits in their daily workflows.
Time Savings and Efficiency
AI soap notes can cut your post-session documentation time from 15-20 minutes down to 2-3 minutes. Instead of spending hours each evening writing clinical notes, you get structured documentation ready within minutes of ending a patient encounter.
- Faster insurance claim processing with consistently formatted notes
- Reduced administrative burden means more energy for your clients
- Late-night documentation sessions become a thing of the past
Many therapists report getting 1-2 hours back in their day, which directly translates to either seeing more clients or having better work-life balance. This approach helps save time while maintaining quality patient progress records.
Consistency and Quality
AI soap notes eliminate the variability that comes with manual documentation. You get the same professional formatting whether it’s your first session of the day or your eighth.
- Every note follows proper soap format automatically
- Critical safety information and treatment plan details are consistently captured
- Better compliance with insurance and regulatory requirements
The technology ensures you’re not missing relevant details when you’re tired or rushed between patient visits.
Best AI SOAP Note Tools for Therapists
Here’s your detailed breakdown of the top AI soap note tools designed specifically for mental health professionals.
Supanote - Built Specifically for Mental Health
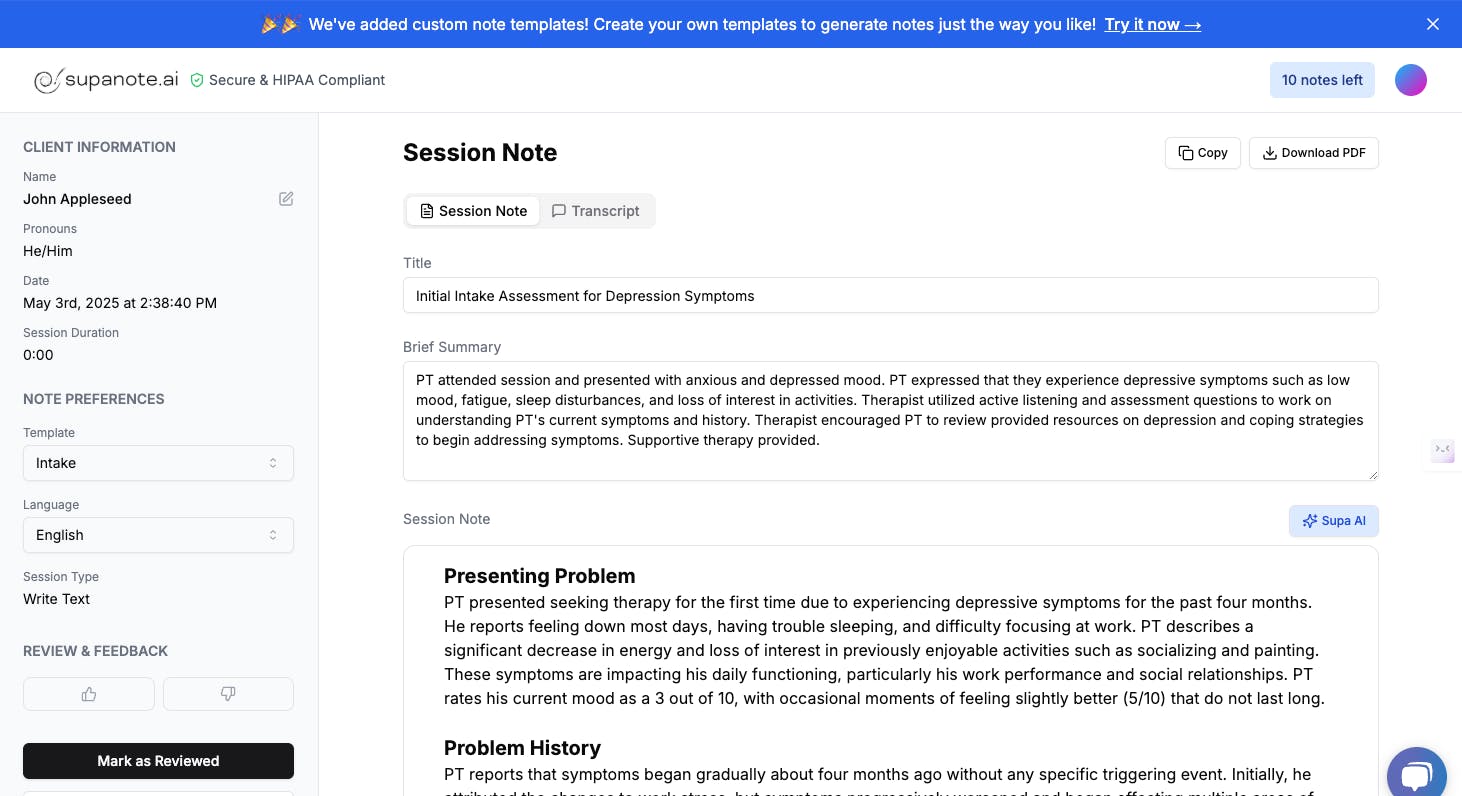
Supanote stands out as the only soap note AI tool built from the ground up specifically for mental health practitioners. It seamlessly integrates directly into your existing EHR system with its signature “Super Fill” button.
- Native EHR integration eliminates copy-paste workflows entirely
- Deep personalization learns and adapts to your unique writing style over time
- Works directly inside SimplePractice, Valant, TherapyNotes, and other major EHRs
- Real human support team understands mental health workflows and challenges
- HIPAA compliant with enterprise-grade security features
Pricing: Starting at $29.99/month billed annually for 40 notes, with 14-day free trial and 20% annual discount
Best suited for: Therapists who want seamless EHR integration and personalized note generator functionality

Mentalyc - Mental Health Focus with Custom Workflows
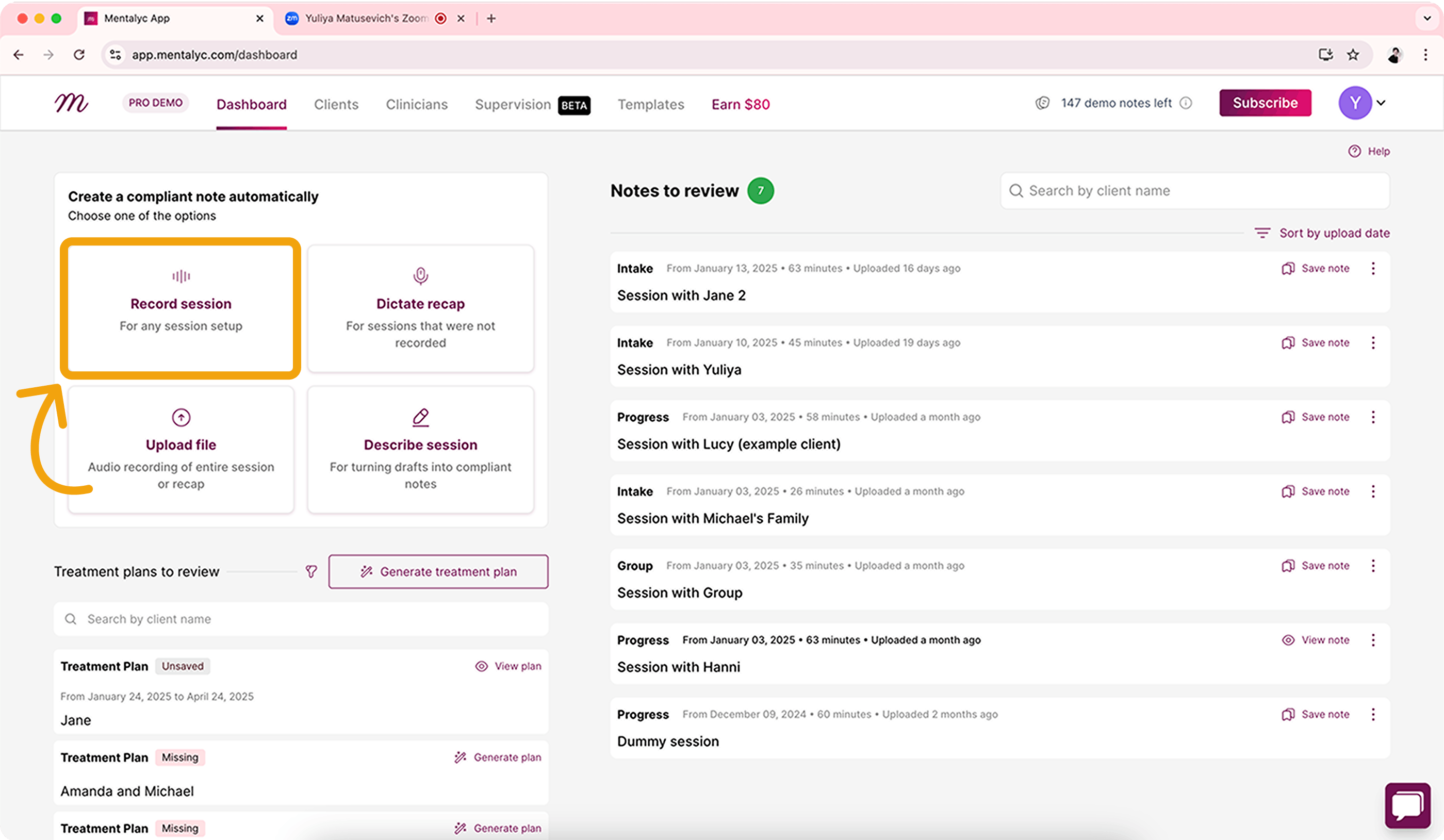
Mentalyc offers robust note templates and team collaboration features that make it ideal for group practices and mental health clinics. The platform provides both SOAP note and DAP note formats to match your clinical documentation preferences.
- SOAP note and DAP notes template options for flexible documentation styles
- Team plans with collaboration features for group practices
- Copy-paste workflow that works with any EHR system
- Bulk processing capabilities for high-volume practices
- Mental health-specific language models trained on therapy terminology
Pricing: Mini plan at $19.99/month for 40 notes, with 16.7% annual discount (2 months free)
Best suited for: Group practices and therapists who need team collaboration features for patient encounters
Upheal - Free Tier with Premium Features
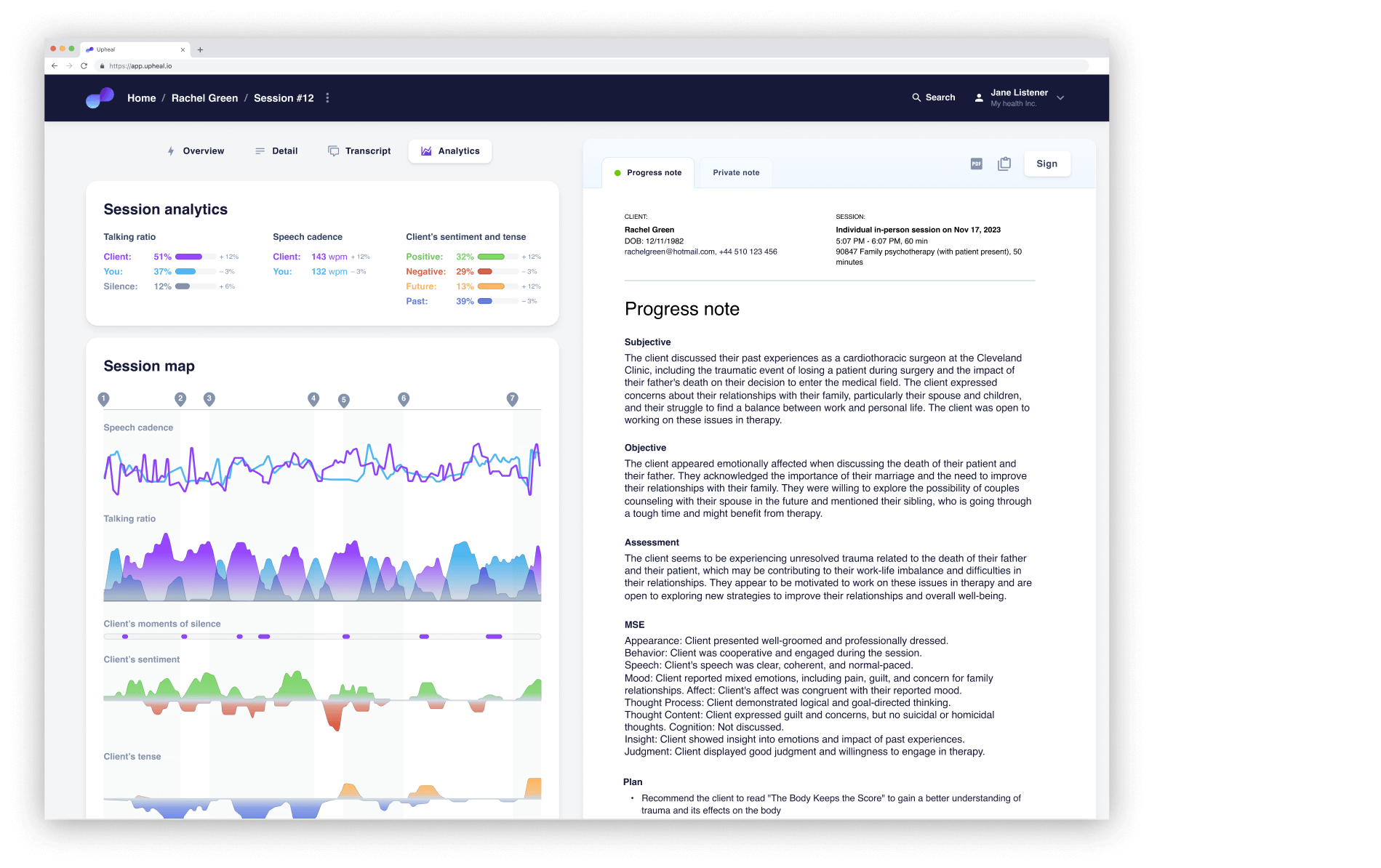
Upheal’s generous free tier makes it attractive for new practitioners or those testing AI medical scribe technology. The platform combines SOAP note generation with built-in telehealth capabilities and session recordings analysis.
- Unlimited clinical notes on permanent free plan
- Built-in telehealth platform eliminates need for separate video conferencing
- Session analysis provides insights into therapy patterns and patient progress
- Automatic session recordings transcription with speaker identification
- Integration with major EHR systems through copy-paste workflow
Pricing: Free tier with unlimited clinical notes, Premium plans start at $19/month with 20% annual discount
Best suited for: New practitioners, budget-conscious healthcare providers, or those wanting telehealth integration
Blueprint - Session-Based Pricing Model
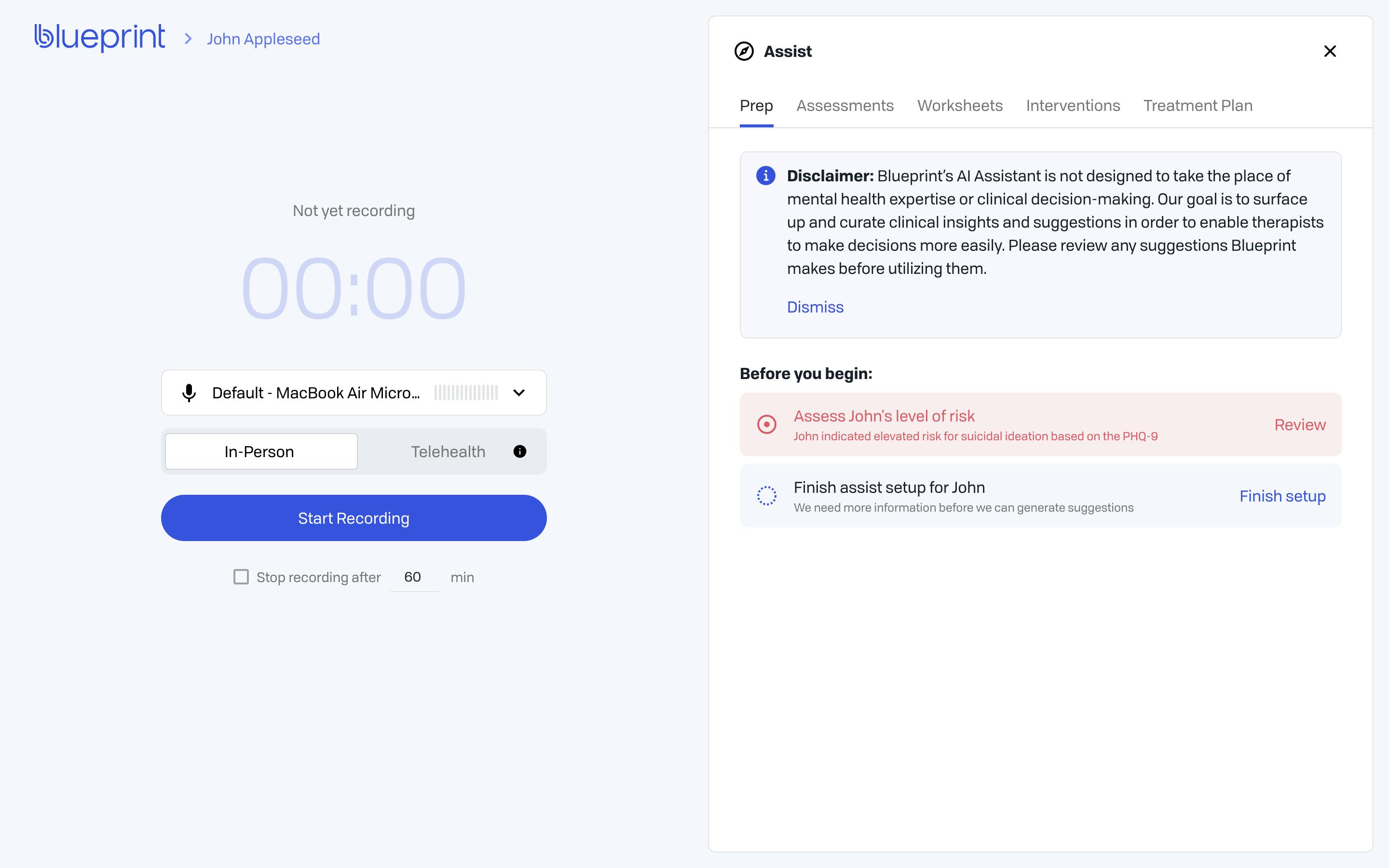
Blueprint recently launched version 2.0 with enhanced AI SOAP notes capabilities and maintains a unique session-based pricing structure. The platform automatically upgrades your plan based on usage to prevent service interruptions.
- Session-based pricing model scales with your practice volume.
- Auto-upgrade system prevents workflow disruptions from usage limits.
- Blueprint 2.0 features improved AI generated SOAP notes accuracy and faster processing.
- Integration with popular EHR systems through secure API connections.
- Specialized note templates for different therapy modalities.
Pricing: Starting at $29/month, with 50% promotional pricing available for first 3 months
Best suited for: Variable-volume practices and healthcare professionals who prefer predictable session-based costs
Quill Therapy Notes - Summary-Based Approach
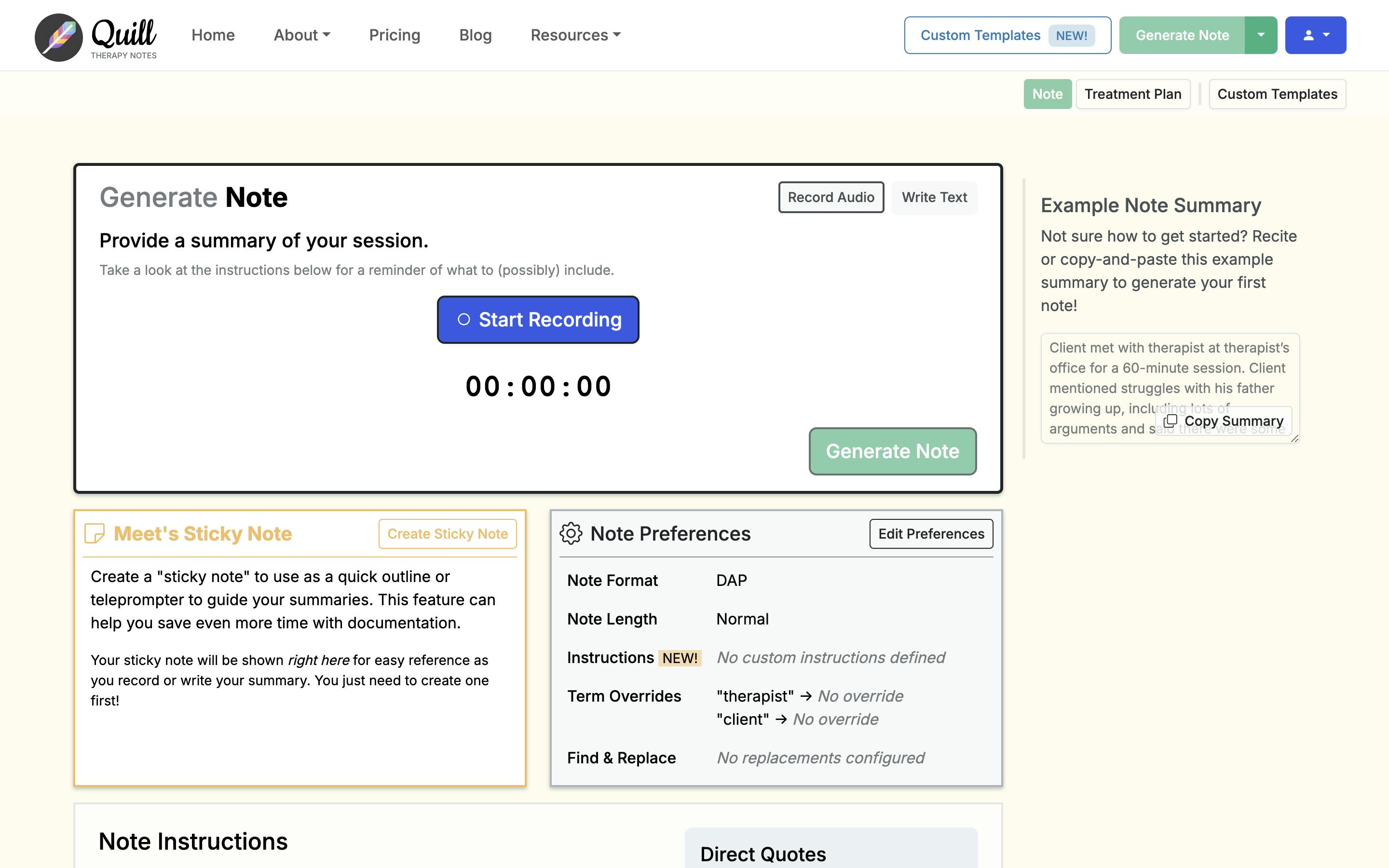
Quill takes a unique approach by generating detailed SOAP notes from session summaries rather than requiring full session recordings. This method appeals to therapists who prefer not to record therapy sessions or work in settings where recording isn’t practical.
- No session recordings required - works from brief session summaries
- Unlimited notes for flat monthly fee provides predictable costs
- Quick turnaround time with generated soap note creation in under 2 minutes
- Customizable note templates match your clinical documentation style preferences
- Privacy-focused approach minimizes audio data storage
Pricing: $20/month for unlimited notes with 14-day free trial
Best suited for: Therapists who prefer summary-based medical documentation or can’t record sessions
Yung Sidekick
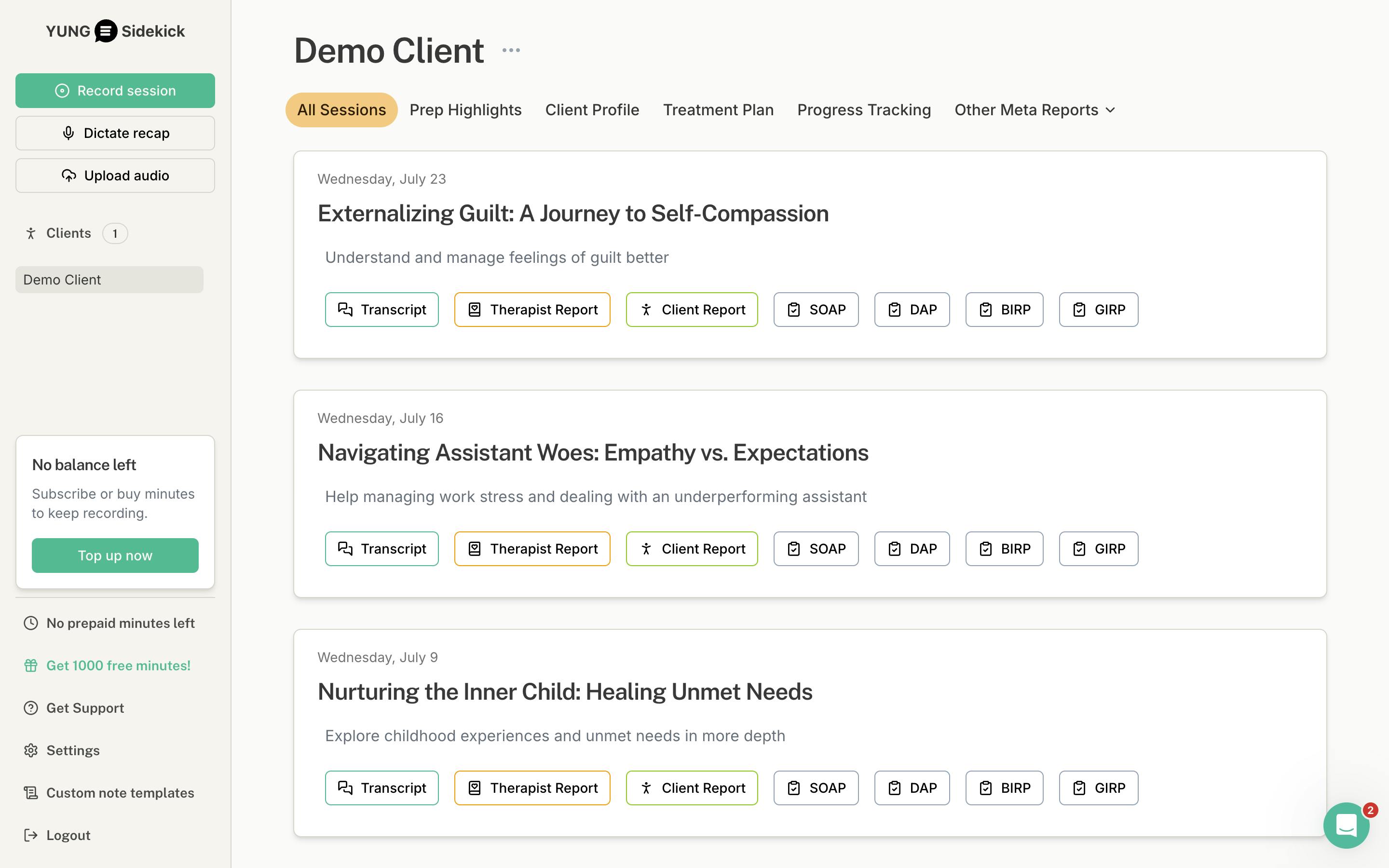
Yung Sidekick operates on a per-session pricing model with overage charges, making it suitable for mental health professionals who want to pay exactly for what they use. The platform focuses exclusively on mental health documentation to serve healthcare professionals.
- Per-session pricing model with transparent overage rates
- Mental health-specific AI tools trained on therapy language and concepts
- Session recordings with automatic speaker identification
- Integration capabilities with major EHR platforms
- Real-time SOAP note generation during or immediately after patient encounters
Pricing: $39.99/month for 130 sessions, overage at $0.03/minute, 7-day free trial with 10% annual discount
Best suited for: High-volume mental health professionals who want usage-based pricing transparency
Freed.ai - Medical-Grade AI for All Specialties
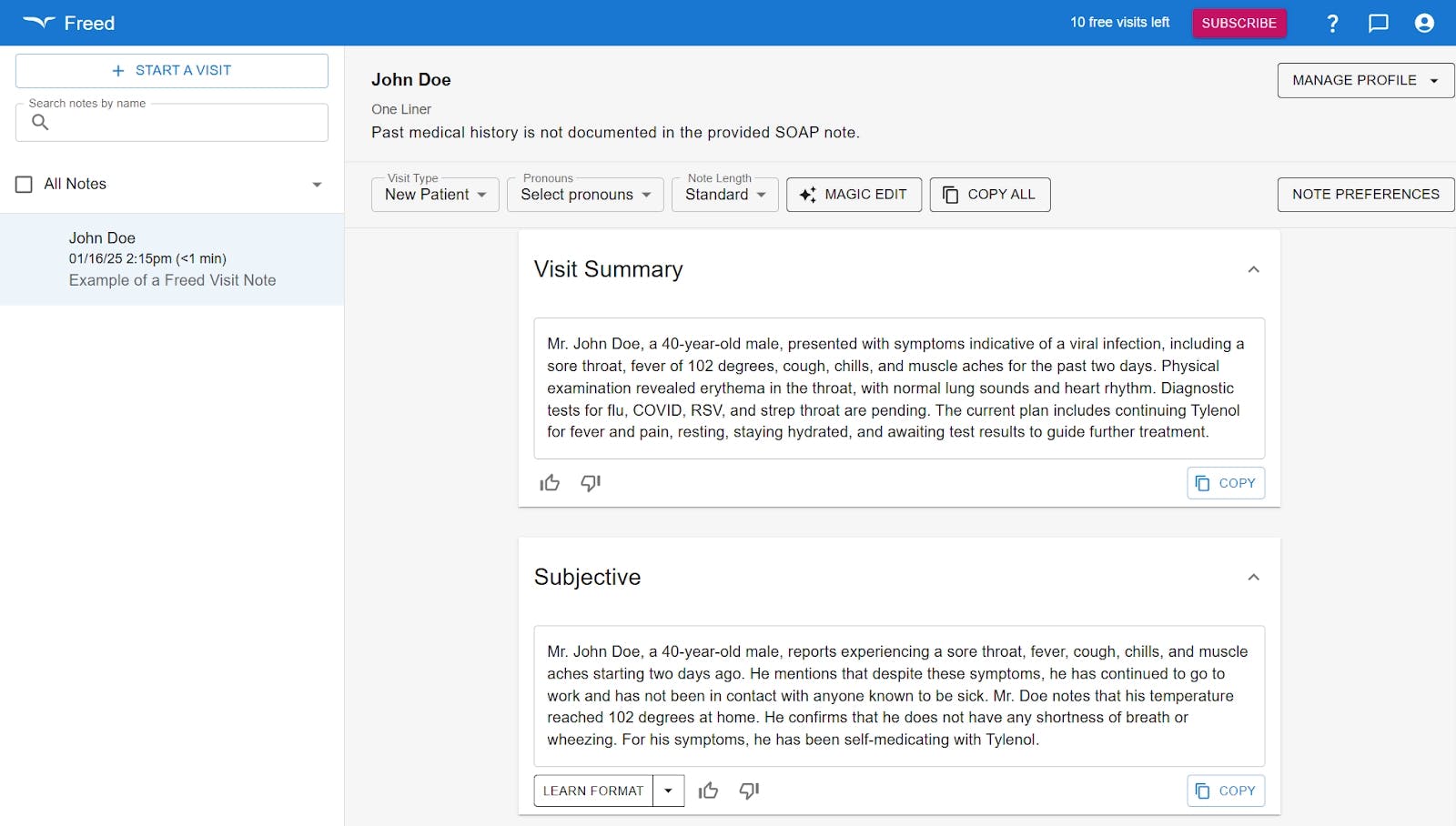
Freed.ai serves the broader medical community but includes robust mental health capabilities. The platform offers unlimited clinical notes at a higher price point, making it suitable for busy practices.
- Unlimited clinical notes and therapy sessions for flat monthly fee
- Works across all medical specialties with mental health-specific note templates
- Enterprise-grade security and hipaa compliant features
- Group pricing available for practices with multiple healthcare professionals
- Advanced AI medical scribe models with high accuracy rates for clinical documentation
Pricing: $99/month for unlimited use, group pricing at $84/month (2-9 users), 10 free visits to start
Best suited for: High-volume practices, multi-specialty clinics, or mental health professionals who need unlimited usage
Autonotes - Multi-Specialty with Mental Health Support
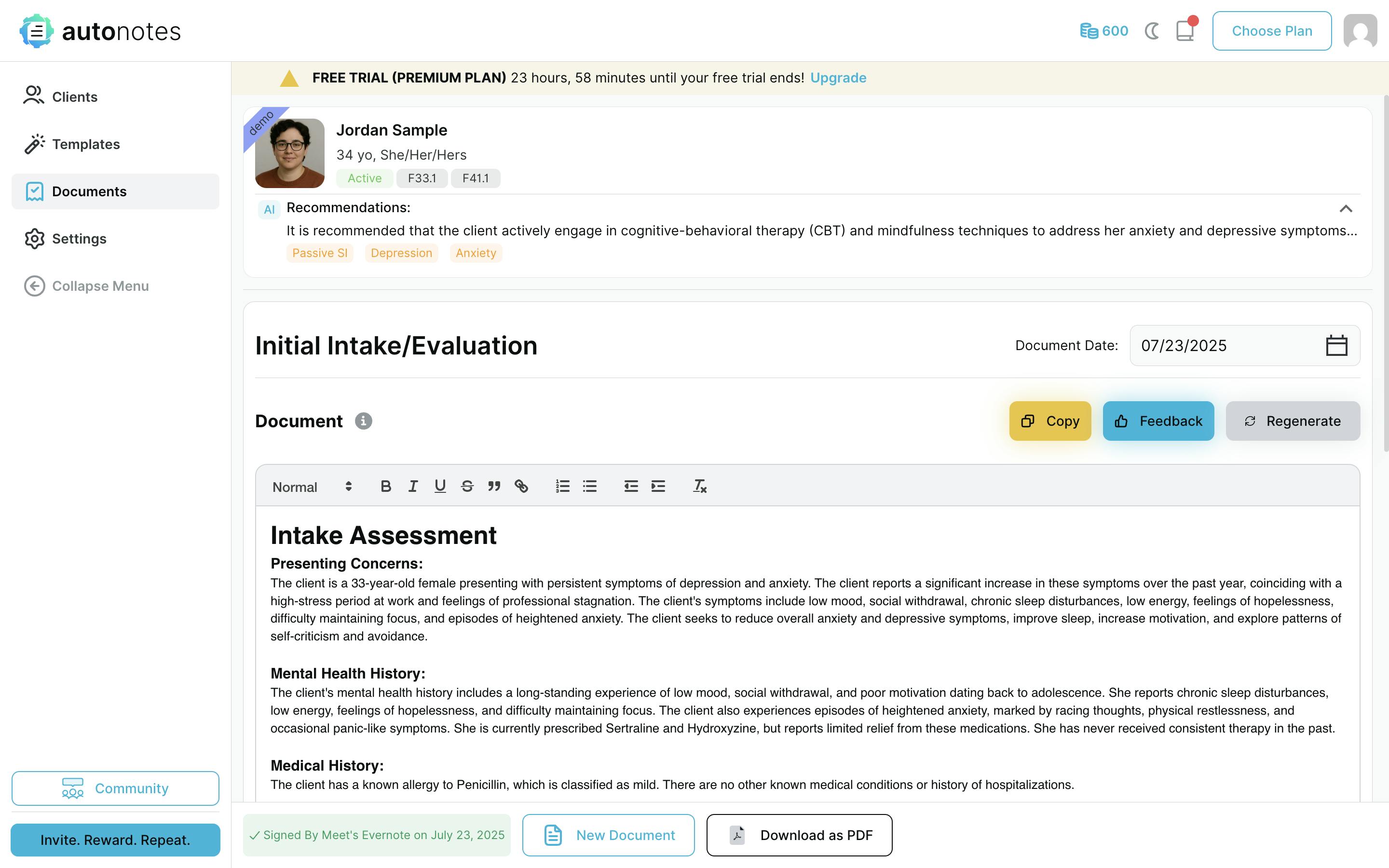
Autonotes uses a credit-based pricing system and serves over 65,000 healthcare professionals across multiple medical specialties. The platform includes specific mental health note templates and PHI de-identification features.
- Credit-based pricing system provides flexible usage options
- Large user base of 65K+ healthcare provider network provides platform stability
- PHI de-identification features enhance privacy protection for patient encounters
- Multi-specialty focus with dedicated mental health note templates
- 24-hour unlimited trial allows thorough testing of the SOAP note generator
Pricing: Starting at $25/month credit-based system, 15% annual discount, 24-hour unlimited trial
Best suited for: Mental health professionals who want flexible credit-based pricing and proven platform reliability
AI SOAP Note Tools Comparison
Here’s a quick overview of the top AI SOAP note tools for mental health professionals, comparing their starting prices and what makes each tool unique for different practice needs.
Tool | Starting Price | Best For |
|---|---|---|
Supanote | $19.99/month billed annually | Mental health practices needing native EHR integration |
Mentalyc | $19.99/month | Teams wanting custom SOAP/DAP workflows |
Upheal | Free (unlimited basic) | Therapists wanting free tier with telehealth features |
Blueprint | $29/month | Session-based pricing with auto-upgrade system |
Quill Therapy Notes | $20/month | Practices preferring summary-based note generation |
Yung Sidekick | $39.99/month | High-volume practices with session-based needs |
Freed.ai | $99/month | Multi-specialty practices beyond mental health |
Autonotes | $25/month | Large practices needing PHI de-identification |
When choosing an AI SOAP note tool, consider your EHR system compatibility, practice volume, and whether you need mental health-specific features versus general medical documentation capabilities.
Key Factors to Consider When Choosing an AI SOAP Note Tool
Choosing the right AI soap notes tool can dramatically impact your daily workflow and practice efficiency. Focus on these critical factors to find the best fit for your specific needs as healthcare professionals.
EHR Integration vs. Copy-Paste Workflow
Native EHR integration saves significant time by placing detailed SOAP notes directly into your system. Tools like Supanote work inside SimplePractice, Valant, and TherapyNotes with their Super Fill button for seamless clinical documentation.
Copy-paste workflows require switching between applications, adding 2-3 minutes per soap note generated and increasing workflow disruption for healthcare provider efficiency.
Pricing Models That Make Sense
Evaluate whether unlimited plans or per-note pricing fits your patient visit volume. Unlimited plans like Quill Therapy Notes at $20/month work well for high-volume practices managing multiple patient encounters daily.
Per-note models like Mentalyc’s $19.99/month for 40 notes suit lower-volume mental health professionals. Take advantage of free trials—most offer 7-14 days to test the note generator functionality.
Mental Health vs. General Medical Focus
Specialized mental health AI tools understand therapy-specific language and workflows better than general medical ai generated soap notes systems. Tools like Supanote, Yung Sidekick, and Upheal offer therapy-specific note templates and terminology for effective documentation.
Their support teams also understand mental health clinical documentation requirements, providing more relevant assistance when issues arise during your documentation process.
Frequently Asked Questions
Q: Are AI generated soap notes HIPAA compliant?
A: Most reputable ai soap notes tools are HIPAA compliant and use encrypted data transmission for patient care documentation. Always verify HIPAA compliance in the tool’s documentation before use. Look for Business Associate Agreements (BAAs) that outline how your patient encounters data is protected.
Q: How accurate are AI generated soap notes compared to manual clinical notes?
A: AI soap notes typically maintain high accuracy for standard clinical documentation elements. However, healthcare professionals should always review and edit generated soap note content before finalizing. The soap note generator serves as a starting point that you can customize to match your clinical judgment and patient care standards.
Can I use a soap note AI generator if my EHR isn’t supported?
Yes, many AI soap notes tools offer copy-paste workflows that work with any EHR system for clinical documentation. While this requires an extra step compared to native integration, it still helps healthcare providers save time. Note generator tools like Supanote, Mentalyc and Quill work well with this approach for mental health professionals.
Q: Do I need to record therapy sessions to use AI soap notes?
Not all SOAP note generators require session recordings for clinical notes. Some work from written summaries or bullet points you provide about patient encounters. However, tools that use recordings typically produce more detailed soap notes and better document patient encounters. Always obtain proper client consent before recording therapy sessions.
Q: What happens if the soap note AI tools generates incorrect information?
Healthcare professionals remain fully responsible for reviewing and correcting any AI generated soap notes content before submitting clinical documentation. Most note generator tools allow easy editing and learning from your corrections. Think of soap note ai as an assistant that needs your professional oversight for patient care.
Q: How much time can I realistically save with AI soap notes?
Most mental health professionals report saving 10-20 minutes per patient visit on clinical documentation. This typically reduces note taking time by 50-75% compared to manual methods. The exact time you save depends on your current documentation process speed and the soap note generator learning curve.
Q: Are there free soap note ai options available?
Yes, Upheal offers unlimited clinical notes on their free tier with basic AI soap notes functionality. Most other note generator tools provide free trials ranging from 7-14 days. Free options often have limitations, so evaluate whether they meet your full patient care needs.
Q: Can AI tools handle specialized therapy approaches like CBT or DBT?
Many soap note generators can adapt to various therapeutic modalities through customization and learning from your corrections in clinical notes. Mental health-focused AI soap notes tools like Supanote and Mentalyc are specifically designed to understand therapy-specific language and interventions for better patient care documentation.
Q: What if I practice in multiple locations or use different devices?
Most AI soap notes tools are cloud-based and accessible from any device with internet connection for seamless clinical documentation. This makes them ideal for healthcare professionals who work in multiple locations or prefer mobile note taking. Check device compatibility during your trial period with the soap note generator.
Conclusion
AI soap notes offer significant time savings and improved clinical documentation consistency for mental health professionals. The right soap note generator depends on your EHR system, practice size, and note taking workflow preferences.
Note generator tools with native EHR integration and mental health-specific focus typically provide the smoothest experience for patient care documentation. Consider starting with free trials to test how well each soap note ai fits your clinical notes style and patient encounters needs.
The investment in ai generated soap notes often pays for itself through increased efficiency and reduced administrative burden. Healthcare professionals who implement these soap note generators report better work-life balance and more time for direct patient care.
Choose a soap note ai that integrates well with your existing documentation process. The best ai soap notes tools will adapt to your writing style while maintaining compliant soap notes standards for all patient visits.