If you’ve ever looked at the clock after your last therapy session and realized you still have hours of SOAP notes to finish, you know the frustration. Documentation is essential for patient care and insurance, but it’s also one of the biggest sources of burnout for mental health professionals.
This is why many therapists are now turning to AI SOAP note generators. But with so many options, each claiming to be the best, it can feel overwhelming to figure out which one truly fits your practice.
So, how do you know which is the best AI SOAP note generator?
It comes down to three factors:
- Workflow fit – Does it integrate with your current EHR or require manual copy-paste?
- Note quality – Does the AI produce structured clinical notes with subjective and objective findings, clinical impressions, and treatment plans you can actually use?
- Value – Do the pricing model and features align with your patient volume and documentation process?
With that in mind, let’s dive into the top AI SOAP note tools available for mental health professionals and healthcare providers in 2026.
What Are AI SOAP Notes?
AI SOAP notes are professional notes created automatically using artificial intelligence. AI SOAP note tools generate structured SOAP notes from therapy sessions or patient interactions.
The SOAP format follows a structured form of four key sections:
- Subjective: Patient’s description of symptoms, history of present illness, and concerns.
- Objective: Observable behaviors, physical exam findings, and vital signs.
- Assessment: Clinical impressions, diagnosis, and clinical decision making.
- Plan: Treatment plans, interventions, and follow-up steps.
SOAP notes provide a consistent way to document therapy sessions and patient visits while meeting clinical guidelines and legal and insurance requirements.
Why Mental Health Professionals are using AI SOAP Note generator?
The shift isn’t just about adopting new technology; it’s about solving a real pain point.
For mental health professionals, hours spent on clinical notes mean less time for patient care, more late-night charting, and greater risk of burnout. AI SOAP note generators change this by giving therapists a faster, more reliable way to document patient encounters.
Here’s what that looks like in practice:
- Save Time: Documentation that once took 20 minutes can now be finished in 2–3 minutes.
- Improve Quality: Structured SOAP notes ensure subjective and objective findings, assessments, and treatment plans are captured consistently.
- Enhance Care: Less time spent documenting therapy sessions means more energy for patient care and mental health treatment.
- Stay Compliant: AI-generated SOAP notes reduce errors and align with clinical documentation standards for audits and insurance reimbursement.
How AI SOAP Note Generators Work
At their core, AI SOAP note tools combine speech recognition, natural language processing, and structured templates to convert therapy sessions into usable documentation.
The process usually looks like this:
- Capture: Through session recordings, dictation, or written summaries.
- Process: The AI extracts relevant information, the patient’s description, objective findings, and clinical impressions.
- Organize: Information is placed into the structured SOAP format automatically.
- Review: You finalize the polished SOAP note, ensuring accuracy and clinical decision-making align with your judgment.
The result? Generated notes that save you time while still producing comprehensive SOAP notes tailored to your workflow.
Top 5 AI SOAP Note Generator Tools for Therapists in 2026
Finding the right tool depends on your practice type, patient volume, and whether you prioritize EHR integration, cost savings, or flexibility. Below are the leading options mental health professionals and healthcare providers are using this year.
1. Supanote – Built Specifically for Mental Health
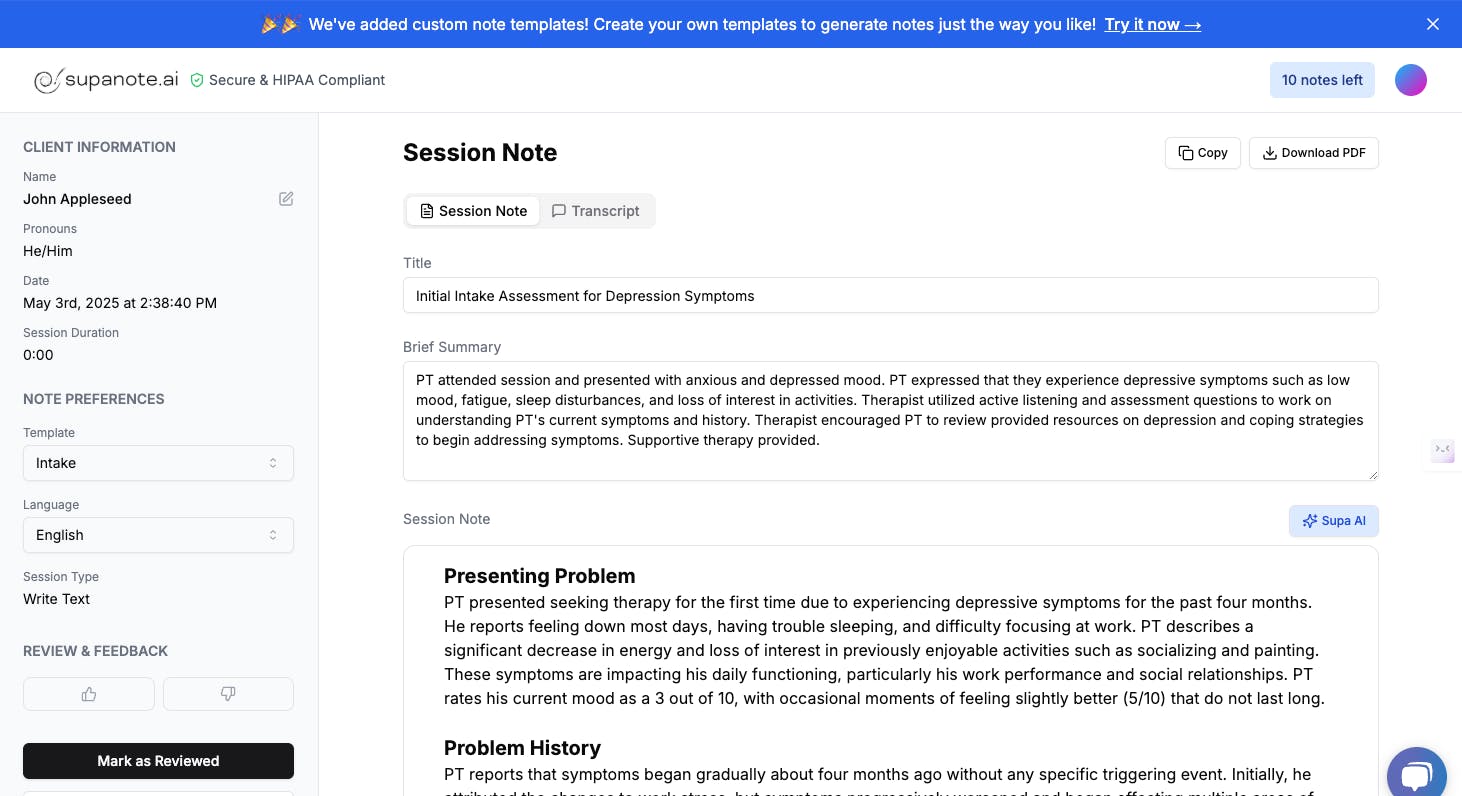
Supanote is one of the few AI SOAP note generators created specifically with mental health practitioners in mind. Its standout feature is the “Super Fill” button, which places AI-generated notes directly into your EHR, removing the need for copy-paste.
- Direct EHR integration saves time and streamlines workflows
- Personalized AI adapts to your writing style and clinical voice
- Compatible with major EHRs like SimplePractice, Valant, and TherapyNotes
- Backed by a real support team trained in mental health documentation needs
- HIPAA-compliant with enterprise-level data security
Pricing: Plans start at $19.99/month (annual billing) for 40 notes, with a 14-day free trial and 20% off annual subscriptions.
Best For: Therapists looking for smooth EHR integration and a note generator that feels tailored to their practice.
2. Blueprint – Flexible Session-Based Pricing
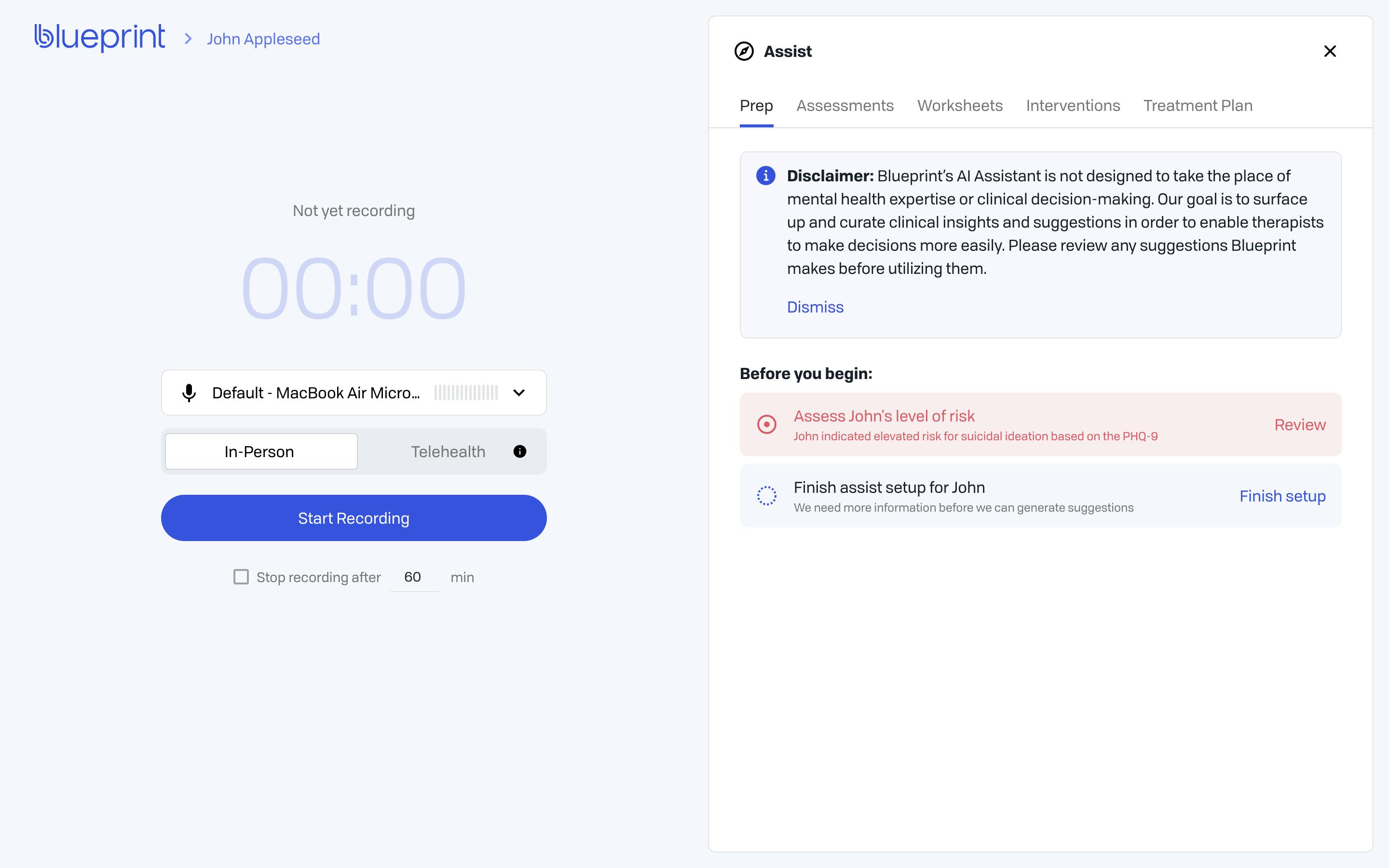
Blueprint’s new version 2.0 brings sharper accuracy and faster processing for AI-generated SOAP notes. What makes it stand out is its session-based pricing model, which adjusts automatically with your caseload so you never hit usage caps or risk workflow interruptions.
- Pricing that scales with your practice volume
- Automatic plan upgrades to avoid service disruptions
- Enhanced SOAP note generation with improved accuracy in v2.0
- Secure API connections for integration with leading EHR platforms
- Specialized templates designed for different therapy approaches
Pricing: The Standard plan starts at $0.49 per session, Plus $0.99 per session, Pro $1.49 per session.
Best For: Practices with fluctuating caseloads and providers who want predictable, session-based costs.
3. Mentalyc – Flexible Notes with Team Collaboration
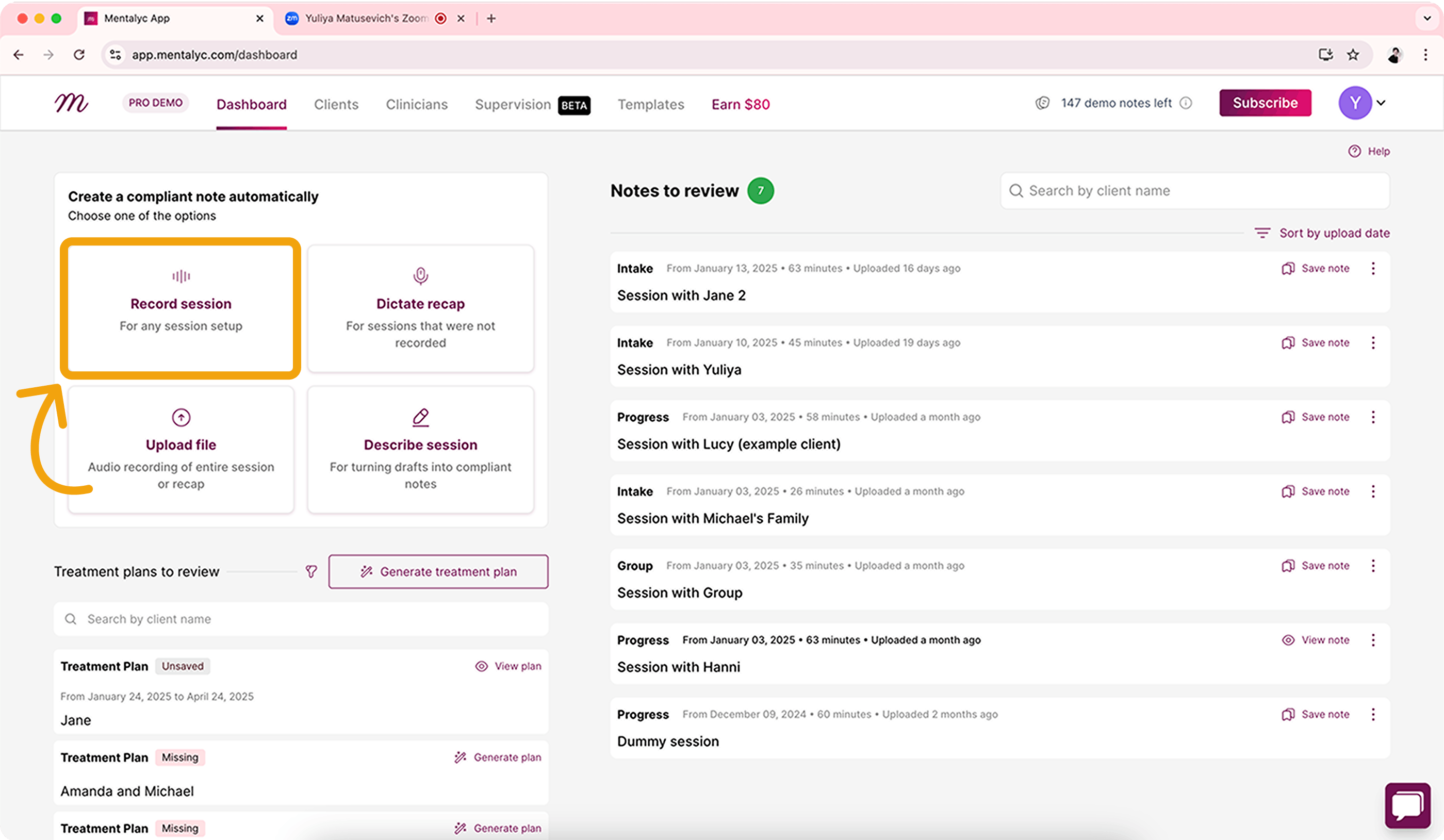
Mentalyc is built with group practices and clinics in mind, offering versatile note templates and collaboration tools. It supports both SOAP and DAP formats, giving therapists the flexibility to document in the style that best fits their clinical workflow.
- SOAP and DAP note templates for customizable documentation
- Team plans with collaboration features for multi-clinician practices
- Copy-paste workflow compatible with any EHR
- Bulk processing designed for high patient volumes
- Mental health–focused AI language model trained on therapy terminology
Pricing: Starts at $19.99/month for 40 notes (Mini plan), with an annual option that gives two months free.
Best For: Mental health clinics and group practices that need collaboration and flexible documentation formats.
4. Upheal – Free Plan with Telehealth Integration
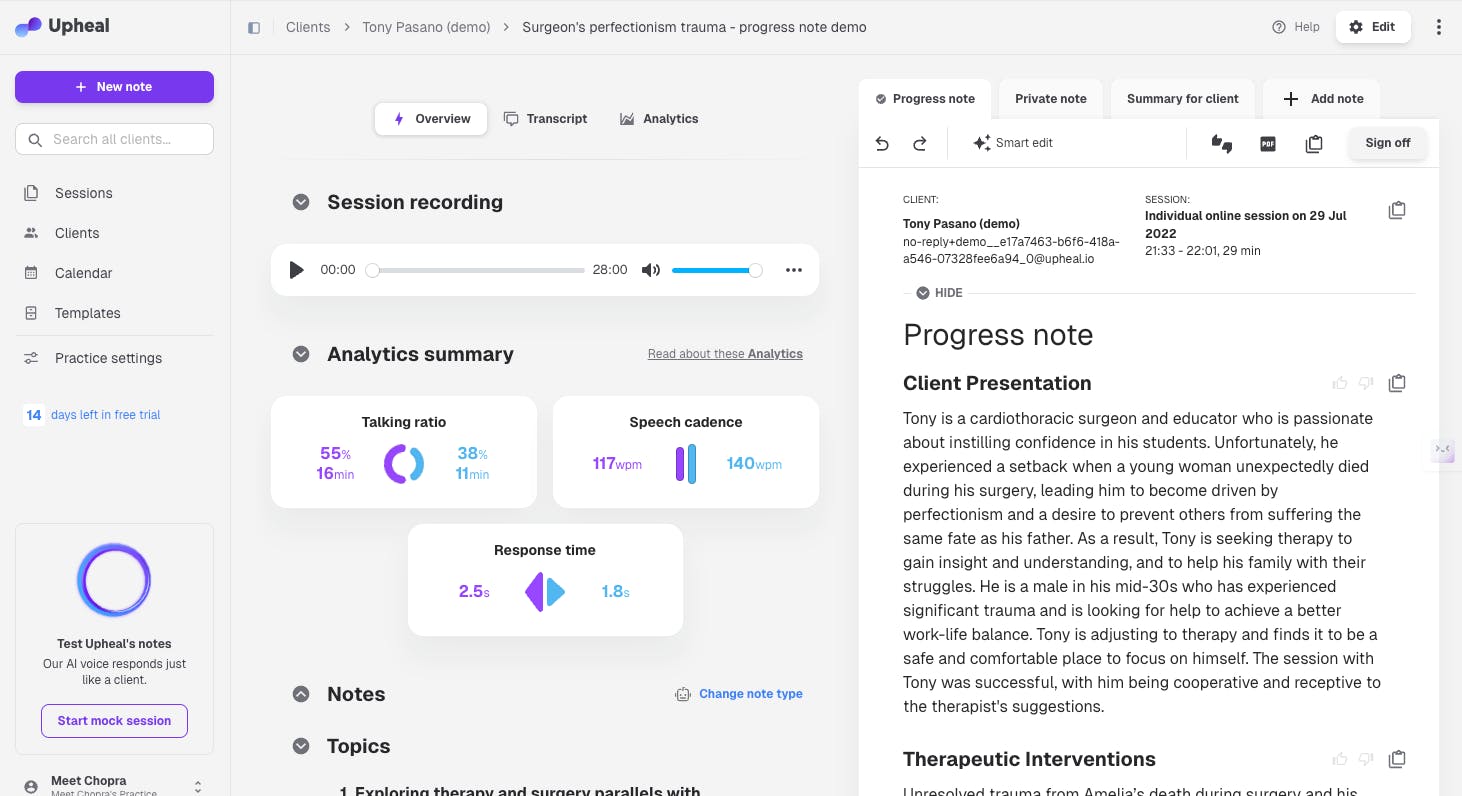
Upheal stands out for its permanent free tier, making it especially appealing to new practitioners or anyone exploring AI medical scribe tools. Beyond SOAP note generation, it doubles as a telehealth platform with built-in video conferencing and session analytics.
- Unlimited clinical notes included in the free plan
- Integrated telehealth eliminates the need for third-party video tools
- Session analysis highlights therapy patterns and tracks client progress
- Automatic transcription of session recordings with speaker identification
- Compatible with major EHRs through a copy-paste workflow
Pricing: Free plan with unlimited notes available; premium plans start at $19/month with 20% off on annual billing.
Best For: Early-career therapists, budget-conscious providers, or those looking for a combined telehealth and SOAP note solution.
5.Freed.ai – Unlimited Notes for Multi-Specialty Practices
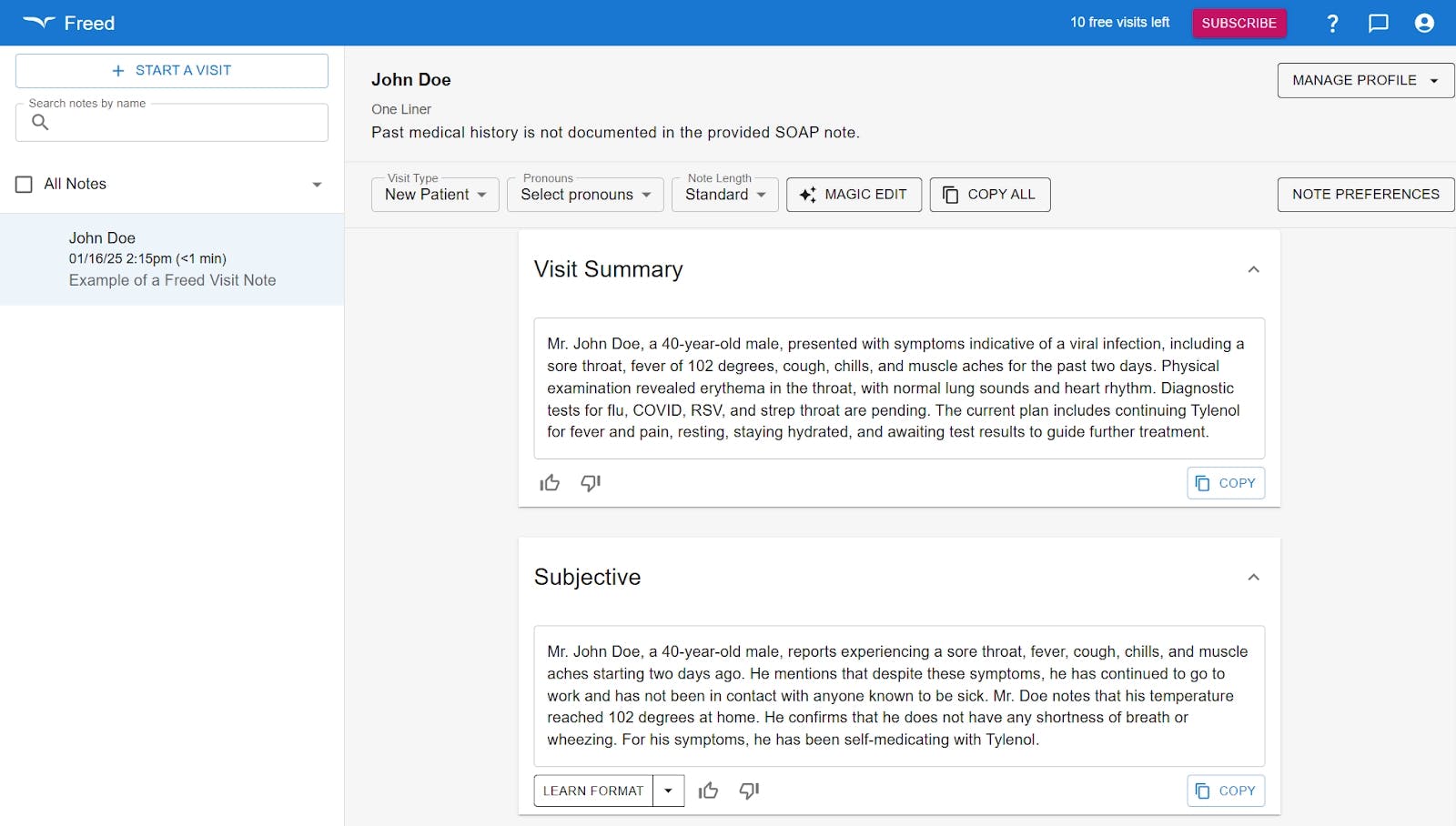
Freed.ai is designed for the wider medical field while still offering strong mental health support. Its standout feature is unlimited clinical notes - ideal for busy practices that don’t want to worry about usage caps.
- Flat monthly fee covers unlimited SOAP notes and therapy sessions
- Serves multiple medical specialties with dedicated mental health templates
- HIPAA-compliant with enterprise-grade security safeguards
- Discounted group pricing available for teams of multiple providers
- Advanced AI medical scribe models ensure high accuracy in clinical documentation
Pricing: $99/month for unlimited use; group plans start at $84/month (2–9 users). Includes 10 free visits to test the platform.
Best For: High-volume practices, multi-specialty clinics, or mental health professionals who need unlimited, reliable documentation.
Quick Comparison Overview
Here’s a quick overview of the top AI SOAP note generators for mental health professionals, comparing their starting prices and what makes each tool unique for different practice needs.
Tool | Starting Price | Best For |
|---|---|---|
Supanote | $29.99/mo | Seamless EHR integration for mental health |
Blueprint | $29/mo | Practices with fluctuating caseloads |
Mentalyc | $19.99/mo | Group practices needing SOAP + DAP flexibility |
Upheal | Free | Early-career or budget-conscious providers |
Freed.ai | $99/mo | High-volume or multi-specialty practices |
Key Factors to Consider When Choosing
When deciding on the best AI SOAP note generator for your practice, focus on these key areas:
- EHR Integration vs. Copy-Paste: Native integration (like Supanote’s Super Fill) saves the most time, while copy-paste adds steps.
- Pricing Models: From free SOAP note options (Upheal) to unlimited clinical notes (Freed.ai), choose a plan that matches your patient volume.
- Specialization: Mental health–focused tools (Supanote, Mentalyc) understand therapy language better than general medical documentation systems.
- Recording Requirements: If you don’t want to use session recordings, consider Mentalyc (summary and DAP workflows).
- Compliance: Always confirm HIPAA compliance, protected health information safeguards, and availability of a Business Associate Agreement (BAA).
Making Your Decision
With so many AI SOAP note generators available, the best choice ultimately depends on your workflow, caseload, and budget.
- If you want high-quality, accurate drafts plus seamless EHR integration and personalised SOAP notes, Supanote is the clear frontrunner.
- For team collaboration and flexible formats (SOAP + DAP), Mentalyc is a great fit.
- For therapists who want more than notes, Upheal combines documentation with built-in session analysis and client engagement tools.
- Practices with fluctuating patient visits may benefit most from Blueprint’s session-based pricing.
- And for large or multi-specialty practices that need unlimited clinical notes, Freed.ai delivers scalability.
No matter which you choose, the goal is the same: reduce the burden of manual documentation, generate compliant SOAP notes consistently, and create more space for meaningful patient care.
FAQs About AI SOAP Note Generators
Q1. Are AI SOAP notes HIPAA compliant?
A. Yes, reputable tools provide HIPAA-compliant SOAP notes. Always request a BAA before using one to document patient encounters.
Q2. Can AI SOAP handle subjective and objective findings?
A. Yes. Most structured SOAP note generators separate patient’s description (subjective) from observable behaviors and vital signs (objective).
Q3. Do I still need to edit AI-generated notes?
A. Yes. AI-generated SOAP notes are drafts, you must review for clinical impressions, treatment plans, and important details.
Q4. Can I use AI SOAP notes without an EHR?
A. Yes. Many work via copy-paste workflows, though EHR-integrated tools save more time.
Q5. Are there free SOAP note options?
A. Yes. Upheal offers a permanent free plan with unlimited clinical notes.
Q6. Can these tools support different modalities (e.g., CBT, DBT)?
A. Yes. Tools like Supanote and Mentalyc adapt to therapy-specific terminology and clinical decision-making.
Q7. Do SOAP note AI tools replace therapists’ judgment?
A. No, they generate structured clinical notes, but clinical decision making remains your responsibility.
Q8. How accurate is Supanote with medical and therapy terminology?
A. Supanote is built specifically for mental health documentation. Its AI is trained to recognize therapy-specific language, clinical impressions, and treatment plans. While the generated notes are highly accurate, you always have the final review to ensure every detail reflects your clinical judgment.
Q9. Can any healthcare professional use Supanote?
A. Supanote was designed primarily for mental health professionals—therapists, psychologists, counselors, and social workers. While other healthcare providers may benefit, Supanote’s workflows, templates, and note styles are optimized for mental health documentation.
Q10. Can ChatGPT write SOAP notes, and how is Supanote different?
A. Yes, ChatGPT can create draft SOAP notes if given session details. The difference is that Supanote is purpose-built for healthcare providers, it is HIPAA-compliant, integrates with your EHR, and adapts to your clinical style, while ChatGPT alone is not designed for medical documentation or patient data security.
Q11. How do I write SOAP notes with Supanote?
A. With Supanote, you simply capture your session (via dictation, summary, or session notes), and the AI generates a structured SOAP note. The Super Fill button then places it directly inside your EHR, eliminating copy-paste.
Q12. Does Supanote offer a free trial?
A. Yes. Supanote offers a 14-day free trial so you can experience AI SOAP note generation and EHR autofill before committing.
Conclusion
AI SOAP note generators are transforming mental health documentation. By turning therapy sessions and patient visits into structured SOAP notes, these tools reduce manual documentation, improve compliance, and give you back time for what matters most- patient care.
For therapists drowning in paperwork, adopting AI SOAP notes isn’t just about efficiency; it’s about creating more space for meaningful patient interactions, protecting patient data, and supporting sustainable mental health care.


