You’re juggling phone calls, referrals, follow-ups, and client crises. Then comes the paperwork- case notes, assessments, service plans. You want to document thoroughly, but who has the time to reinvent the wheel for every case?
That’s where a solid case management documentation template comes in.
Whether you're a licensed clinical social worker, therapist, or case manager, this blog will walk you through what goes into effective case documentation, why it matters, and how a template can save you hours without sacrificing clinical quality.
What Is a Case Management Documentation Template?
A case management documentation template is a structured format for recording key client information- intake data, action plans, service coordination, progress tracking, and follow-up notes.
It's more than just a form; it's an essential part of the case file that helps manage case notes effectively.
Unlike general therapy notes, case management documentation tends to focus on:
- Functional needs (housing, food stamps, finances, safety)
- Resource coordination (referrals, social services, service authorisations)
- Outcome tracking (client's goals met, barriers, follow-up)
It ensures consistency across sessions, improves compliance with health insurance portability regulations (HIPAA and the accountability act), and reduces legal and audit risk.
For agencies using case management software, these templates help streamline workflow and keep documentation in chronological order.
Templates also make it easier to write in a clear, consistent style and help social workers avoid burnout from repetitive documentation tasks.
The right case note templates simplify how you record notes, track progress, and meet deadlines in a timely manner. They also standardise the format used by a team of case managers across departments.
How Case Management Documentation Differs from Progress Notes
While both are essential for client care, case management documentation and progress notes aren’t the same and confusing them can disrupt your workflow (or worse, your audits).
Progress notes are clinical records that capture what happened in the therapy room- the client’s symptoms, the interventions used, their response, and mental health updates. These are typically written by therapists or psychologists to demonstrate medical necessity and track treatment progress.
On the other hand, case management documentation zooms out.
It focuses on the practical side of care: coordinating services, handling referrals, ensuring follow-ups, and tracking progress toward functional or logistical goals (like housing, transportation, or access to resources).
Aspect | Progress Notes | Case Management Notes |
|---|---|---|
Written By | Therapists, psychologists | Social workers, case managers, discharge planners |
Focus | Mental health symptoms, treatment progress, clinical insights | Referrals, social services, coordination of care |
Purpose | Track therapeutic goals and interventions | Ensure follow-up, track logistics, coordinate wraparound support |
Style | Often in-depth, using frameworks like SOAP or DAP | More task-focused, sometimes brief but structured |
Example Line | “Used CBT to challenge cognitive distortions.” | “Client referred to housing authority. Follow-up call scheduled.” |
In short:
Progress notes document treatment. Case notes document movement.
When used together, they create a full picture of your client’s journey- what’s happening inside and outside the therapy room.
Why Case Documentation Matters in Clinical Practice
It’s not just about paperwork - your documentation is the treatment roadmap.
Why it’s essential:
- Supports continuity of care: Clear documentation helps other case managers and social workers stay updated on the client’s case file.
- Protects you legally: If ever questioned, your notes serve as a legal record of services provided and decisions made.
- Ensures funding compliance: Many funders, including Medicaid and managed care plans, require complete and well-organised documentation to justify services.
- Improves treatment outcomes: A structured record keeps treatment goals, client interactions, and next steps visible and trackable.
Accurate note taking isn’t just a formality; it’s a clinical responsibility. Writing case notes in a timely manner ensures decisions and observations are captured accurately.
Additionally, recording case notes helps teams align around client needs, ensure effective communication, and identify evidence of improvement or stagnation.
Comprehensive documentation also plays a major role in risk mitigation. A missed service, overlooked safety concern, or misdocumented referral can put both the client and clinician at risk. The clearer and more detailed your case notes, the stronger your clinical defence and continuity of care.
A complete record, notes not only what was done, but also why it was done- linking decisions to treatment goals and observed behaviours.
Whether you’re working in inpatient care, school-based social work, or community-based social services, clear case documentation is the backbone of quality care.
Core Components of a Case Management Note Template
Here’s what a strong case management template should include:
Section | What to Include |
|---|---|
Client Info | Name, ID, demographics, client details |
Date & Time | Of contact or service |
Type of Contact | In-person, phone, virtual, collateral |
Presenting Issue | Why the client is seeking help |
Services Provided | Referrals made, resources given |
Client Progress | Movement toward goals or barriers |
Follow-up Plan | Next steps, who’s responsible |
Case Manager Notes | Objective observations, the client’s subjective thoughts |
Signatures (if needed) | Staff and/or client acknowledgement |
A consistent structure helps social workers and case managers capture critical client information, reducing the risk of omitting sensitive information that may influence treatment outcomes or legal decisions. It also provides a useful audit trail in the event of supervision, licensure review, or insurance disputes.
You may also choose to add fields like: treatment goals, interventions provided, progress toward goals, and referrals made. These help ensure your note doesn’t just document, but also reflects on effectiveness and plans ahead.
Case Note Template Examples for Different Settings
Example 1: Community-Based Case Manager
Client's Appearance: Neatly dressed, calm, alert.
Client Interaction: Discussed housing options. Provided referral to local shelter.
Progress: Client filled out housing application.
Services Provided: Printed application, bus pass to the housing office.
Next Steps: Follow up in 3 days to confirm submission.
Example 2: School Social Worker
Client: 13-year-old presenting with behavioural outbursts and panic attacks.
Client’s Subjective Thoughts: "Sometimes I feel like I can't breathe when I'm in class."
Objective Observations: Tearful, fidgety, avoids eye contact.
Services Provided: Referred to school counsellor; contacted guardian.
Treatment Goals: Reduce panic symptoms and improve attendance.
Follow-Up Plan: Weekly check-ins for the next 4 weeks.
Example 3: Hospital Discharge Planner
Critical Client Information: Patient has no support system post-discharge.
Client Details: 68-year-old with diabetes, recently hospitalised.
Action Plans: Coordinate in-home nursing visits. Apply for food stamps.
Additional Information: Patient needs medication reminders.
These examples illustrate how templates help document different types of care with clarity, structure, and sensitivity.
Advanced Tips: Documentation in Multi-Provider Teams
When multiple case managers or social workers are involved in a client's care, documentation can easily become fragmented. Here’s how to keep your case file unified:
- Use shared case note templates in your case management software
- Log all case manager interactions- even brief check-ins
- Reference other providers’ notes to show continuity
- Mark all service plan updates with timestamps and authorship
- Differentiate objective observations from interpretation
If you’re coordinating with a mental health provider, primary care physician, or housing coordinator, your documentation becomes the glue that holds the team’s plan together.
How Supanote Helps You Document Smarter
Supanote is designed for mental health professionals who need to get their notes done fast- without compromising clinical quality.
Here’s how Supanote simplifies case management documentation:
- Voice-to-Note: Record your session summary, and Supanote turns it into a complete note- instantly.
- Custom Templates: Choose from SOAP, DAP, or case management templates tailored to your setting.
- Auto-Time Stamping: Every entry is securely tagged with time and date to meet audit and compliance requirements.
- Smart Organization: Notes are saved by client and session in one dashboard- no more hunting through folders.
- HIPAA-Compliant: Your notes are encrypted and stored securely, protecting your clients’ privacy.
- Collaborative View: Share notes with supervisors or team members as needed, with proper permissions.
Whether you're writing 2 notes a day or 20, Supanote adapts to your workflow so you can spend less time documenting and more time supporting your clients.
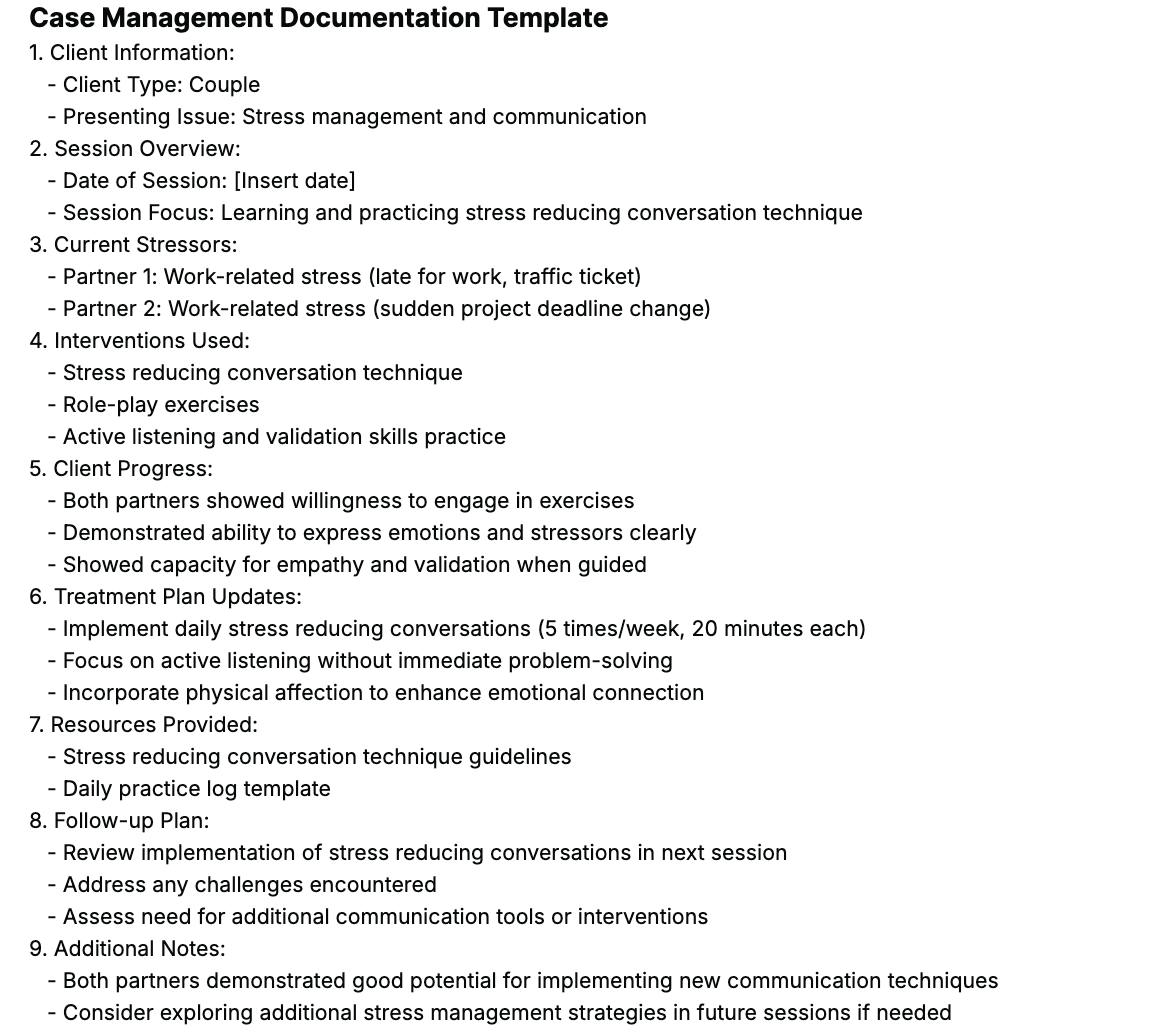
Here's an example of a Case Management Documentation Template created via Supanote
Get Back to Clients, Not Case Notes
Supanote helps you generate clear, professional case documentation in minutes
Try Supanote for Free Today
FAQs
Q. What’s the best format to write case notes for audit-readiness?
A. Use structured templates that include the client’s goals, services provided, referrals, and follow-up plans. Supanote auto-generates these sections for you.
Q. How do I document a client refusing services?
A. Note the refusal. Example: “Client declined referral to psychiatrist. Expressed preference for peer support group.”
Q. Can I use templates across clients?
A. Yes - but always tailor it with the client's appearance, subjective thoughts, and treatment progress.
Q. What’s the difference between case notes and social work case notes?
A. Social work case notes may include deeper therapeutic insights, while case management focuses on logistics, referrals, and care coordination.
Q. How often should I update the client’s record?
A. Every significant interaction—whether it’s a phone call, team meeting, or in-person visit—should be recorded.
Q. What’s a red flag in poorly written case notes?
A. Generic phrasing (e.g., “Client doing okay”) without evidence, services, or next steps.
Q. Do I need to document collateral contacts (like speaking to a family member)?
A. Absolutely. Clarify who you spoke with, what was discussed, and how it relates to the client’s care.
Q. What if multiple team members provide services on the same day?
A. Record each interaction separately. Use your software’s timestamped entries to avoid overlap.
Q. Is it okay to write brief notes?
A. Yes, as long as they’re complete. Cover the who, what, when, and why.
Q. How do I protect a client’s privacy when documenting sensitive information?
A. Avoid speculation. Stick to facts. Use secure systems, and redact when necessary for care coordination.
Q. How do templates help improve treatment outcomes?
A. They promote consistency, reduce errors, and ensure no client detail falls through the cracks.
Q. Can I voice-record and convert it into notes?
A. Yes. With Supanote, you can record sessions and get instant case note drafts that meet clinical standards.
Final Thought
You don’t have to choose between quality documentation and more time with clients. A smart case management documentation template - especially when paired with the right tools- can streamline your process, reduce burnout, and ensure no detail is missed.
If you’re ready to stop dreading your case notes, Supanote can help you record, organise, and auto-generate documentation that’s accurate, audit-ready, and done in minutes.
Ready to try? 10 notes on us!
Login to your Supanote account and instantly access 10 free notes
Get it Now!
Resources for Further Reading
- NASW Standards for Social Work Case Management
- Switchboard: Case Management Documentation Guide
- SAMHSA: Best Practices for Behavioural Case Management
- Medicaid Documentation Standards by State
- HIPAA Compliance for Case Notes
