A long therapy day ends, and you sit down to document.
Suddenly, the memory fades: What exactly did the client report? How did they respond to that CBT intervention? Did we discuss homework for next session?
If you're nodding, you're not alone.
For many mental health professionals, clinical documentation can be one of the most time-consuming and stressful parts of the job.
But, with the right mental health note template, you can make writing progress notes faster, clearer, and more aligned with both legal and clinical standards.
In this guide, we’ll break down how to use mental health note templates to enhance your documentation- without losing the nuance and heart of your work.
What Are Mental Health Progress Notes?
Mental health progress notes are clinical records written by mental health providers after a therapy session. They serve as a legal record and document the client’s mental health progress, symptoms, treatment goals, and the therapist’s clinical observations.
These notes are part of the official medical record, accessible to other healthcare providers and required for insurance claims, audits, and documentation of medical necessity.
A good mental health note captures:
- What the client reported
- How the client responded to therapeutic interventions
- The therapist's observations and clinical reasoning
- The treatment plan and next steps for future sessions
Why Use a Mental Health Note Template?
Using a structured mental health note template can:
- Save valuable time for mental health professionals
- Reduce administrative tasks
- Ensure documentation meets legal and ethical standards
- Improve clarity and track progress across sessions
- Simplify collaboration with other healthcare providers
Note templates also help you stay consistent, especially when balancing complex caseloads, managing risk assessments, and complying with licensing board expectations.

Here's a sample Mental Health Note Template that you can use.
Key Elements to Include in Every Therapy Note
No matter which format you choose, a well-written note should include these essential details:
- Client identification: Name, date, session number
- Presenting issue: What the client presented with in this session
- Subjective reports: Client’s words, emotional state, self-reported symptoms
- Objective observations: Therapist’s observations (e.g., mood, behavior, speech)
- Interventions used: Techniques such as cognitive restructuring, mindfulness techniques, or exposure work
- Client response: How the client responded to interventions
- Treatment plan: Progress toward treatment goals, any changes, and what’s planned for the next session
Sample Template: Supanote-Inspired Note Layout
You can use this template manually or in Supanote’s auto-fill tool.
Supanote Session Note Template
Client Name:
Date:
Therapist:
Session Number:
Type of Session: (individual/family/group)
1. Presenting Concern
Briefly describe what the client presented with in this session.
2. Subjective Reports
What the client reported feeling, saying, or describing.
3. Objective Observations
Therapist’s observable behaviors, physical presentation, tone, affect.
4. Interventions Used
e.g., cognitive restructuring, identifying cognitive distortions, psychoeducation, role-playing
5. Client Response
Did the client respond well? Show resistance? Experience insight?
6. Progress Toward Treatment Goals
Are we moving toward goal completion? Is any revision needed?
7. Plan for Next Session
What’s next? Topics, interventions, homework assignments, referrals.
Some Common Mental Health Note Formats (with Templates)
There’s no single way to write therapy notes. Different formats suit different settings and styles of clinical practice.
Here are the most widely used therapy note templates:
1. SOAP Notes
One of the most popular formats in the mental health field.
S: Subjective
What the client reported (e.g., “Client reports feeling anxious most mornings.”)
O: Objective
What the therapist observes (e.g., “Client appears withdrawn; minimal eye contact.”)
A: Assessment
Clinical impressions, changes since prior sessions, risk assessment, diagnostic considerations
P: Plan
What will be done in future sessions (e.g., introduce new coping strategies, assign homework)
Use when: You want a clear structure for both clinical and insurance documentation.
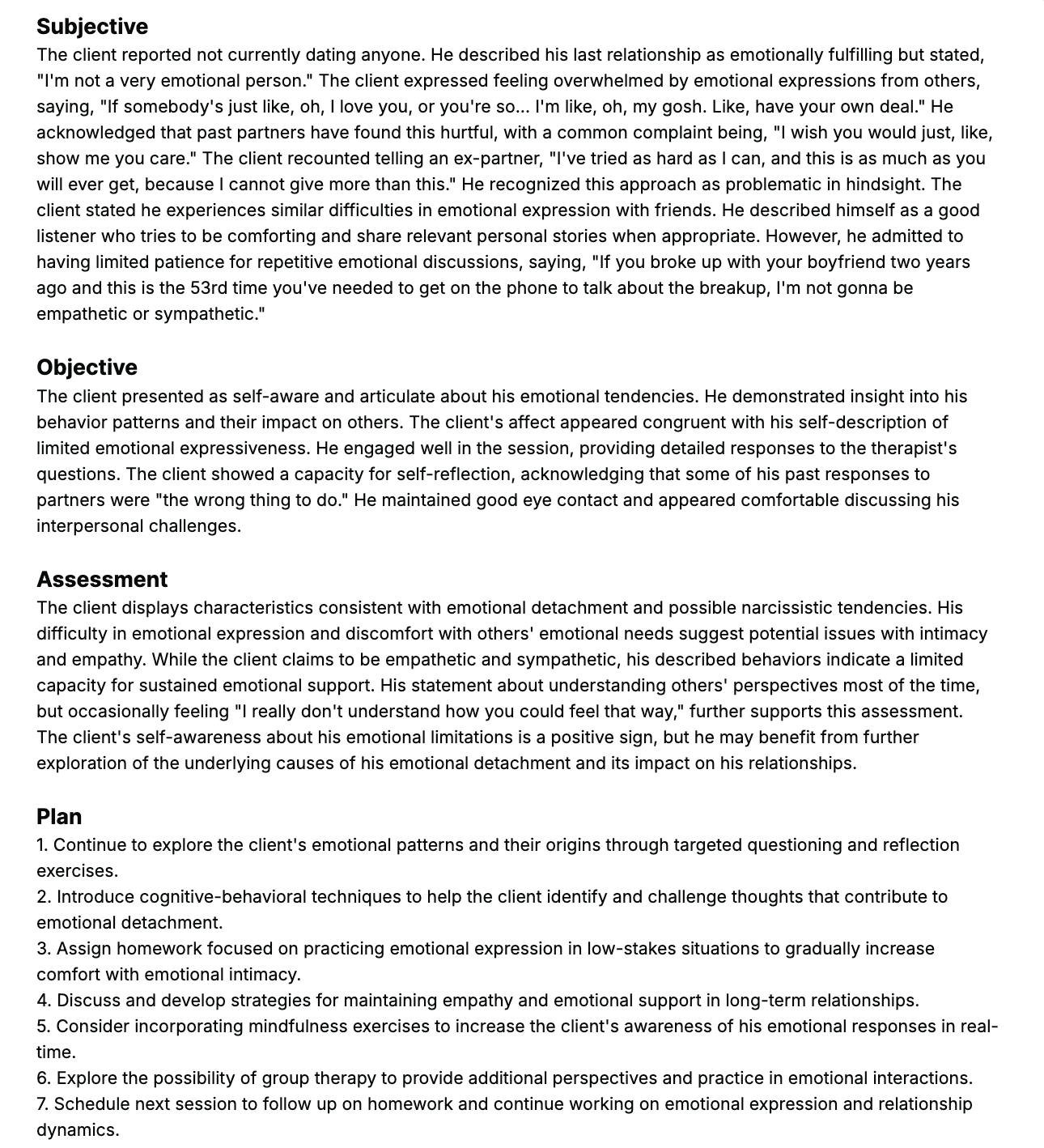
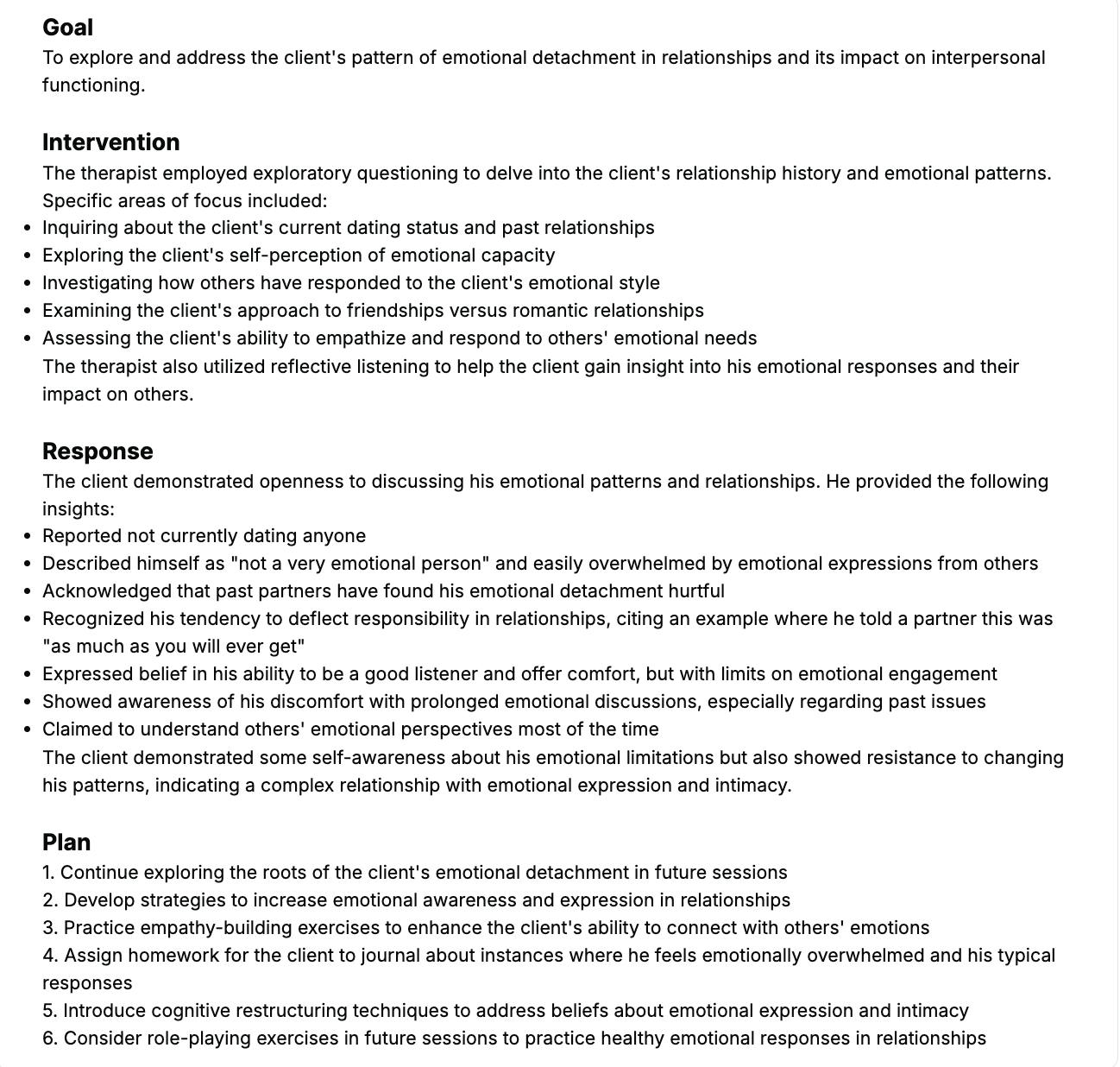
Here's a sample SOAP note created using Supanote.
2. DAP Notes
D: Data
Includes both subjective and objective information.
A: Assessment
Your clinical take on what’s going on.
P: Plan
Next steps, referrals, or continued focus.
Use when: You want a more concise version of SOAP notes.
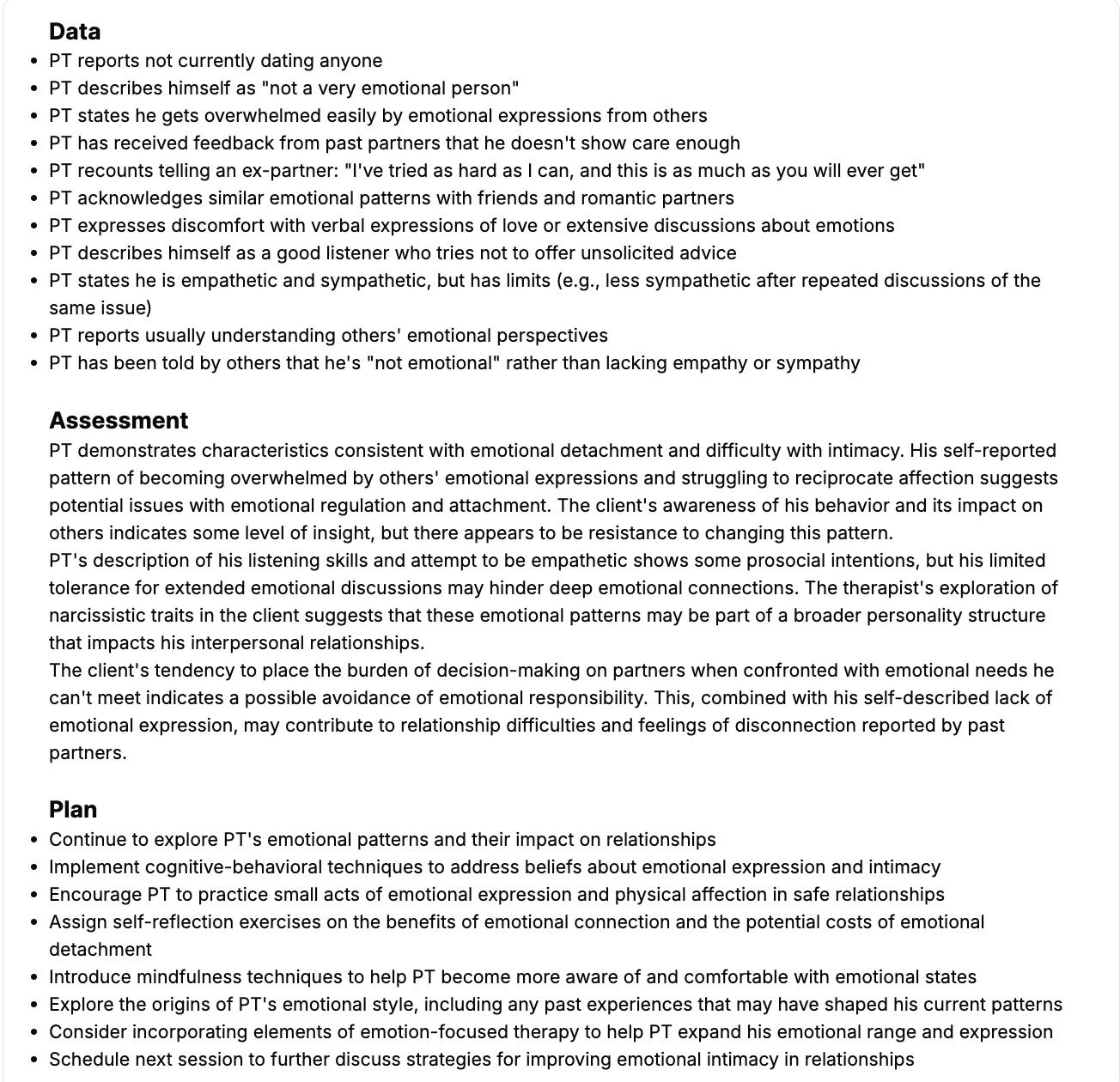
Here's a sample DAP note generated using Supanote.
3. BIRP Notes
B: Behavior
I: Intervention
R: Response
P: Plan
BIRP notes help in tracking client progress session by session in behavioral health settings.
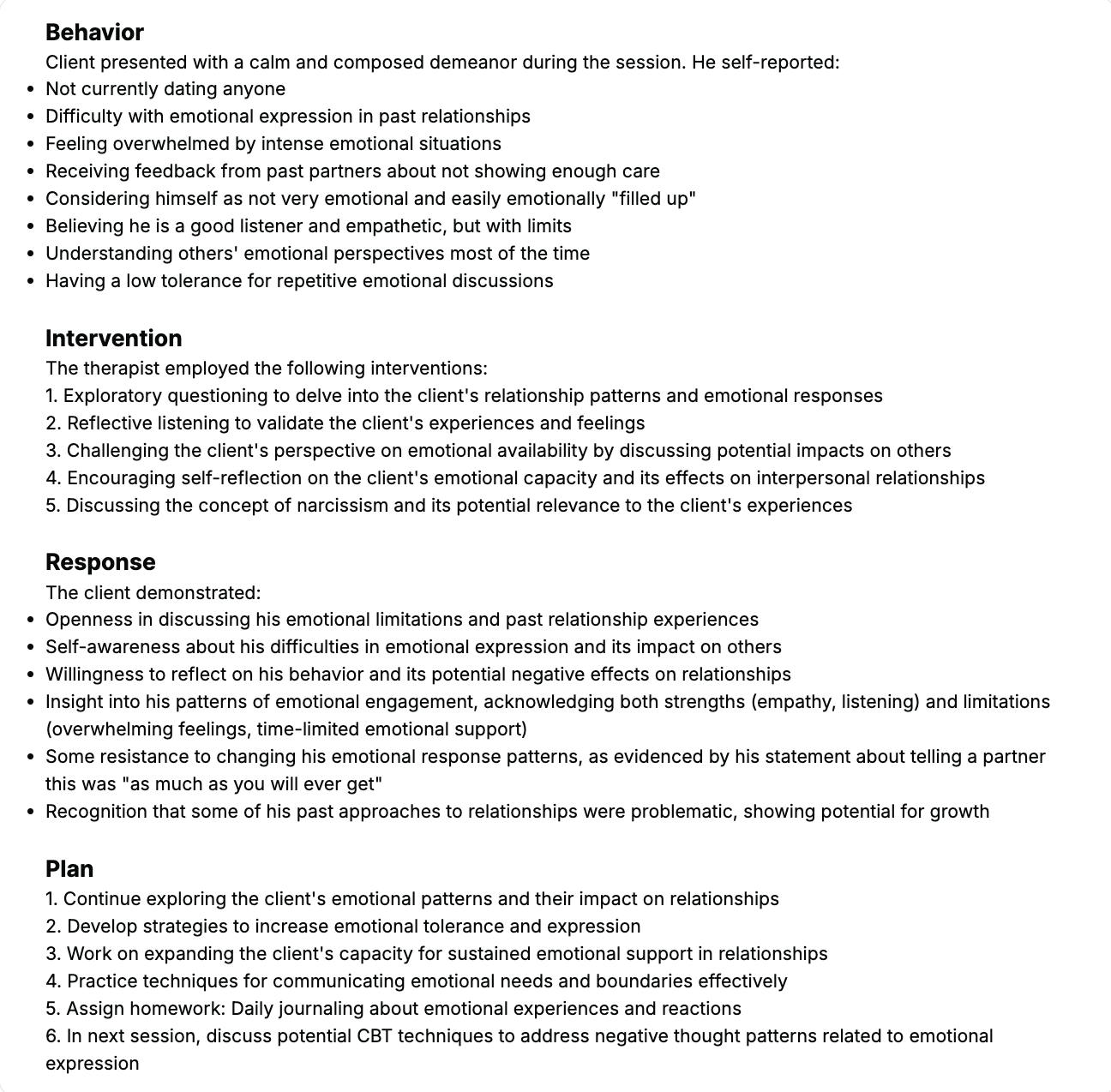
Here's a sample BIRP note generated using Supanote.
4. GIRP Notes
Adds Goals to the format:
G: Goals
I: Intervention
R: Response
P: Plan
Use when: You’re working on measurable treatment goals and need to show alignment with client progress.
Here's a sample GIRP note generated using Supanote.
Best Practices for Writing Progress Notes
Here’s what experienced mental health professionals do to make notes useful, clear, and defensible:
- Write notes immediately after the therapy session
Reduces memory bias and captures more key details - Stick to observable behaviors and clinical data
Avoid vague phrases- note specific client behaviors, mood shifts, and therapy responses - Keep it professional, not personal
Notes are part of the official medical record- write accordingly - Balance detail with efficiency
Don’t transcribe the session. Focus on what’s clinically relevant. - Use note formats that match the session type
E.g., family sessions, group therapy, or trauma-informed care may need specific nuances - Highlight changes in mental health progress
Even small shifts matter when documenting patient progress - Incorporate the treatment plan
Show how interventions connect to treatment goals
Mistakes to Avoid When Writing Mental Health Notes
- Overloading with narrative, skipping structure
- Leaving out risk assessments in high-risk cases
- Forgetting to update progress toward treatment goals
- Copy-pasting from previous sessions without updating client progress
- Skipping client response to interventions
- Writing generic notes that don’t support medical necessity
How AI Tools Can Help You Write Better Notes
Modern practice management software and AI-powered tools like Supanote can significantly enhance your documentation workflow.
Here’s how digital note templates help:
- Provide structured formats that adapt to session type
- Save valuable time with auto-filled session headers and treatment plans
- Remind you to capture objective data and subjective reports
- Help you track client progress over time
- Stay compliant with HIPAA and licensing board standards
Supanote even learns your note style over time, helping you stay consistent while reducing administrative tasks.

Tips for Tracking Client Progress Over Time
- Use consistent note formats across sessions
- Highlight progress on treatment goals
- Reference prior sessions to show trends
- Include direct quotes from client reports
- Compare client appears or behavior changes across weeks
FAQs: Mental Health Note Template
Q1. What’s the best note format for new therapists?
Start with SOAP or DAP, they’re widely accepted and easy to learn.
Q2. Can I reuse note templates across clients?
Yes, the structure, but never copy-paste content. Each client’s mental health journey is unique.
Q3. How do I document if a client was late or silent?
Note it under objective observations or client response (e.g., “Client appeared distracted; minimal verbal engagement.”)
Q4. Do I need to include homework every time?
No, but documenting homework assignments shows intentional clinical planning.
Q5. What if a client misses a session?
Log a no-show note with the date, contact attempts, and plan for rescheduling.
Q6. How do I ensure my notes are HIPAA compliant?
Use encrypted digital tools, store securely, and avoid names in group/family session content.
Q7. Can I include informal language?
Avoid casual tone in therapy notes- use clinical, objective language to meet legal and ethical standards.
Q8. What’s the difference between therapy notes and progress notes?
Progress notes go in the medical record. Psychotherapy notes are private, for your own reflection.
Q9. Can Supanote help me write faster notes?
Yes. Supanote helps mental health professionals write compliant, structured notes using AI—freeing up time to focus on clients.