The right mental health practice software can transform how you deliver client care and manage your practice efficiently. Yet with dozens of options available, choosing the wrong behavioral health software can waste valuable time and disrupt your workflow completely.
This guide breaks down the three main categories of practice management software available today. You’ll discover which AI documentation tools, comprehensive practice management systems, and specialized behavioral health platforms best fit your specific needs and budget constraints.
Understanding Mental Health Practice Software Categories
The mental health software landscape offers three distinct categories. Each is designed to solve different operational challenges in your behavioral health practice.
Three Main Types of Practice Software
- AI-powered documentation and note-taking tools - Focus specifically on streamlining clinical documentation through automated transcription and intelligent therapy notes generation
- Comprehensive practice management systems - Handle all aspects of practice operations including scheduling, billing, client records, and documentation in one integrated platform
- Specialized mental health platforms with integrated features - Combine essential practice management tools with therapy-specific features like treatment plans and outcome tracking
What Each Category Solves
AI documentation tools excel at eliminating the administrative burden of note-writing. They require integration with existing ehr systems though.
They’re ideal when you’re satisfied with your current health ehr but want to dramatically reduce documentation time. These tools help behavioral health professionals focus more on patient care.
Comprehensive systems work best for new practices or those wanting to consolidate multiple tools. However, they may lack the specialized mental health features you need for clinical workflows.
Specialized platforms bridge this gap effectively. They offer practice management basics with therapy-focused workflows for mental health practitioners.
Though they might not match the advanced AI capabilities of dedicated documentation tools. Each system requires careful evaluation of your specific practice needs.
AI-Powered Documentation Tools
AI documentation tools are transforming how mental health professionals handle clinical notes efficiently. These specialized platforms reduce documentation time while maintaining quality and compliance standards for behavioral health practices.
Supanote
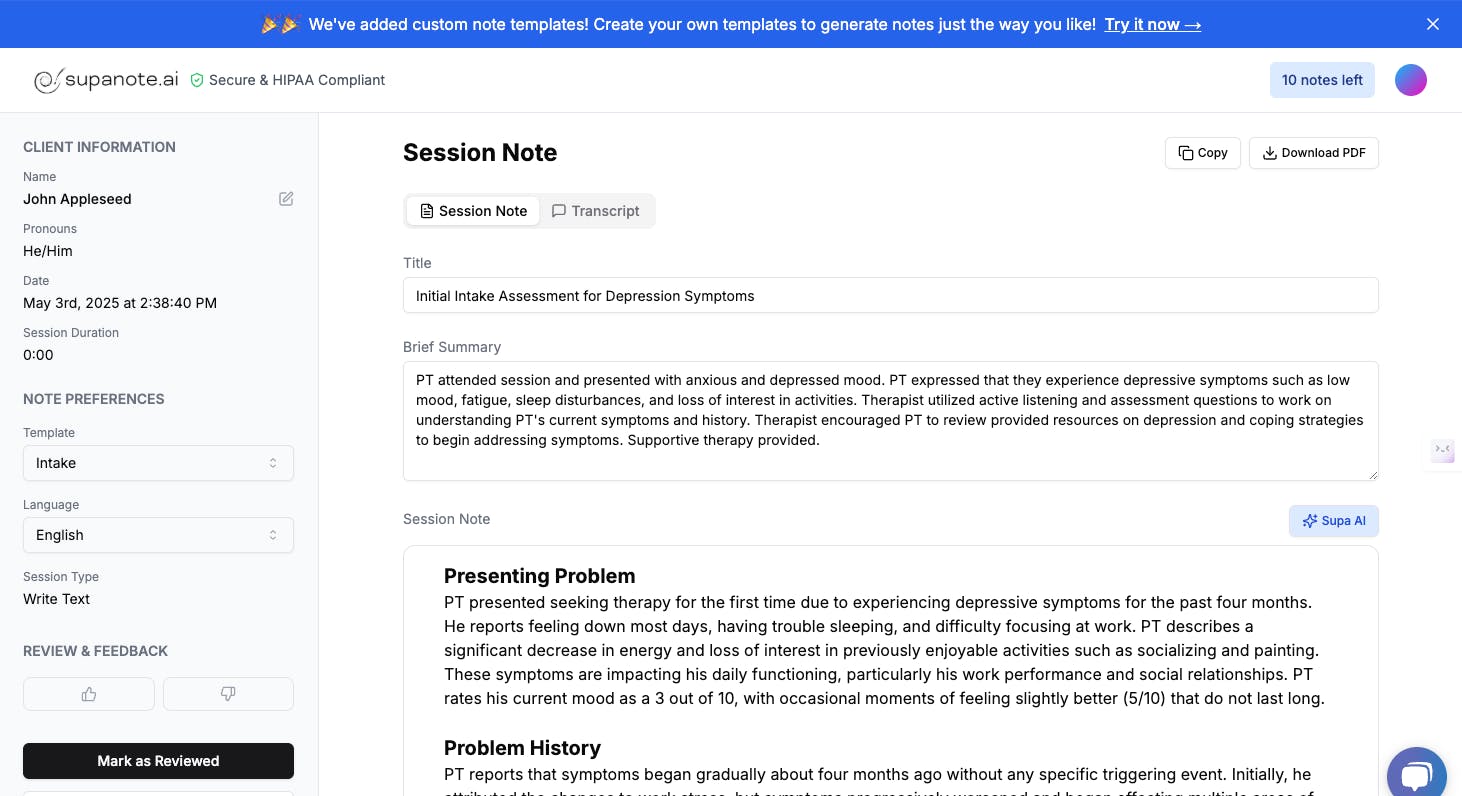
Supanote is designed exclusively for mental health professionals. It offers intuitive tools that align with therapy workflows seamlessly.
The ‘Super Fill’ button provides seamless ehr system integration. It automatically populates your existing system with generated notes for streamlined workflows.
- Deep personalization learns your documentation style
- Native integration eliminates copy-paste workflows
- Therapist-friendly interface designed by healthcare professionals
Pricing: Basic plan starts at $19.99/month for 40 notes, with 14-day free trial
Best suited for: Therapists wanting seamless ehr software integration
Mentalyc
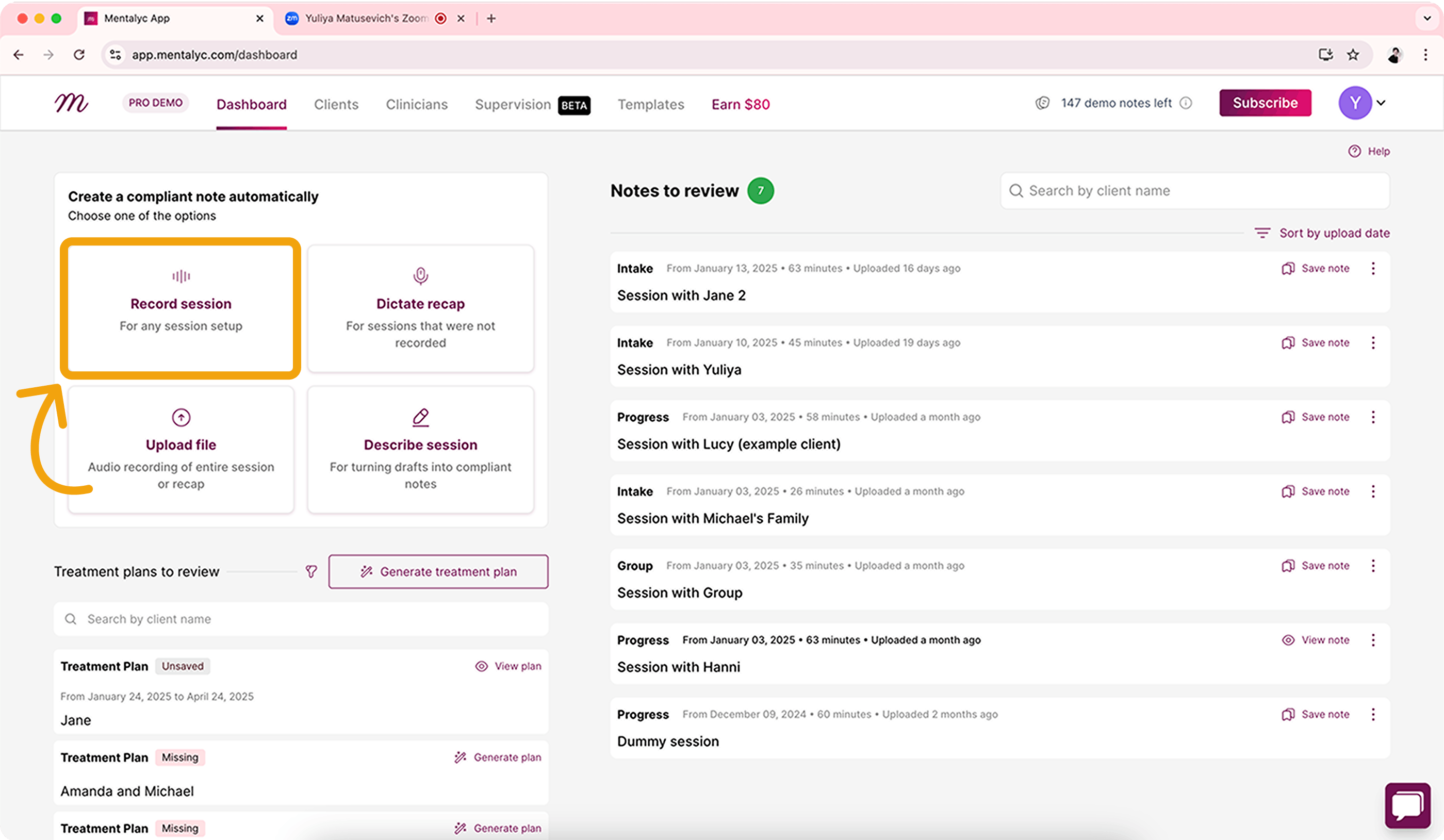
Mentalyc focuses on customizable workflows with robust SOAP and DAP template options. You can easily transfer generated notes to your existing health ehr through copy-paste functionality.
- Custom workflow creation for different therapy modalities
- Comprehensive template library for clinical documentation
- Team discount options available for group practices
Pricing: Mini plan at $19.99/month for 40 notes
Best suited for: Mental health practices needing flexible documentation templates
Upheal
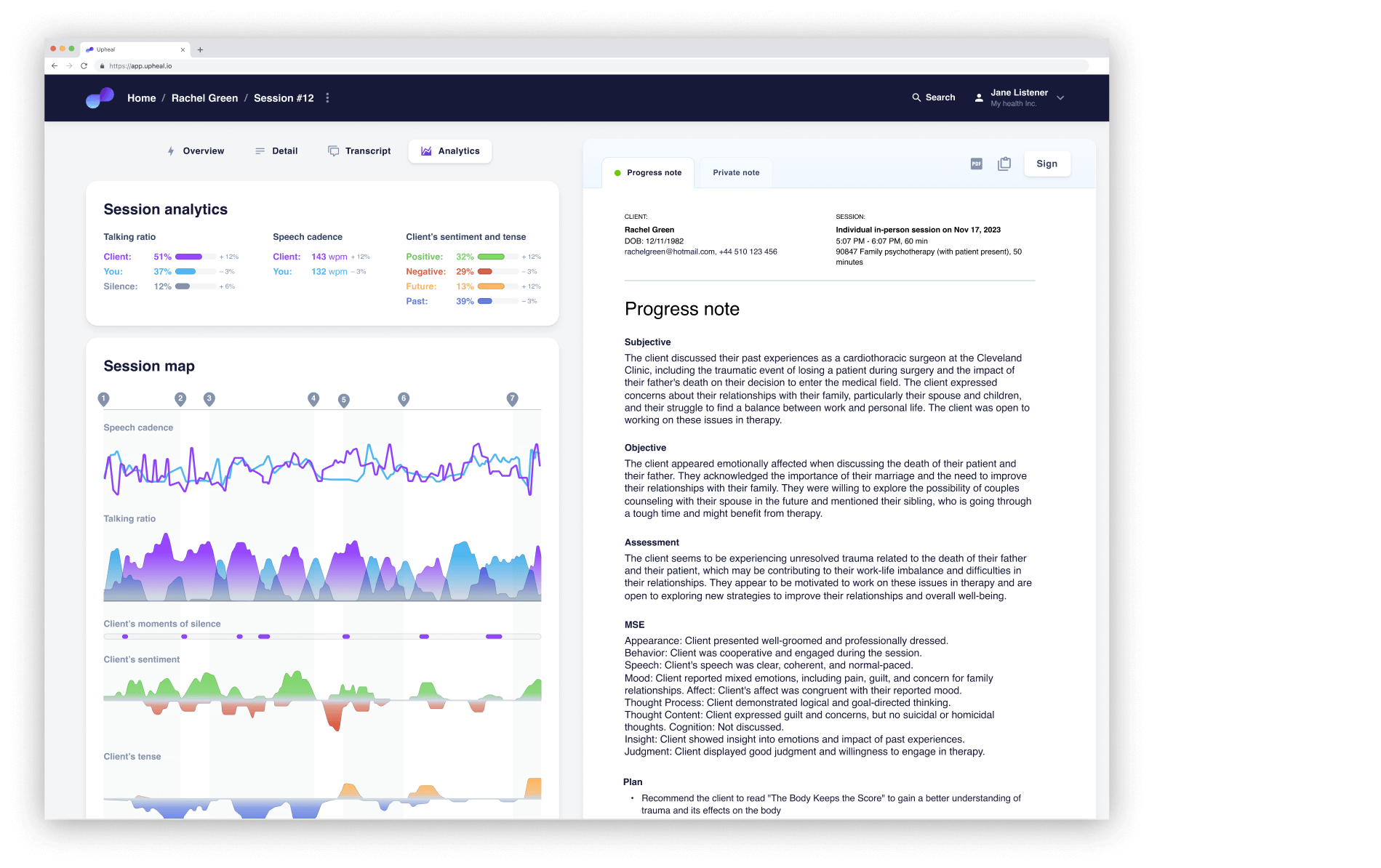
Upheal combines AI documentation with integrated telehealth capabilities and session analysis tools. The unlimited free basic notes tier makes it accessible for mental health professionals trying AI documentation.
- Built-in telehealth platform integration
- Session analysis and insights features
- Permanent free tier for basic notes
Pricing: Plus plan at $19/month for advanced features
Best suited for: Therapists conducting telehealth sessions
Blueprint
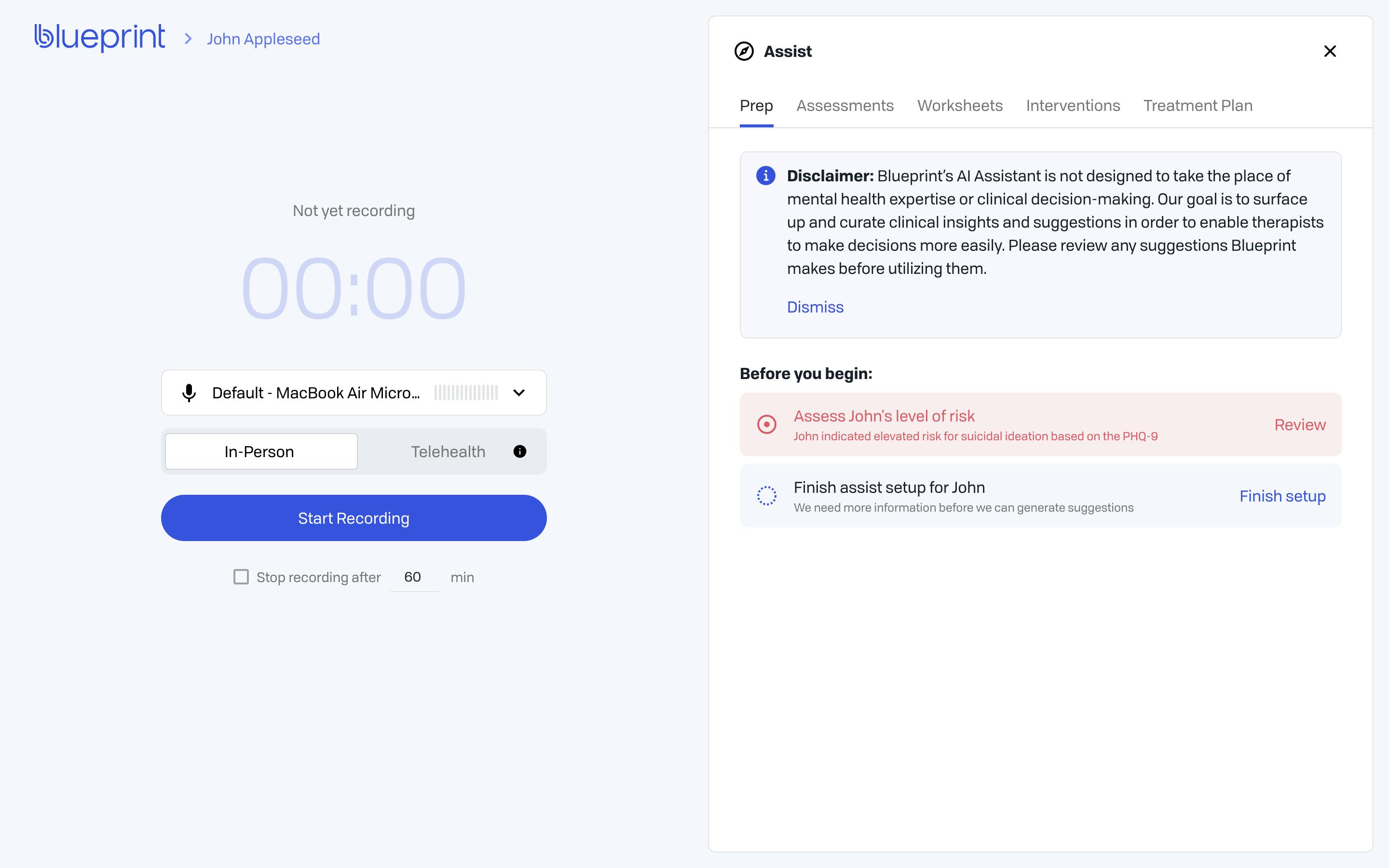
Blueprint uses session-based pricing and recently launched Blueprint 2.0 with enhanced features. The platform auto-upgrades plans based on usage for mental health practices.
- Session-based pricing model
- Recent platform updates and improvements
- Auto-upgrade functionality
Pricing: Starting at $29/month
Best suited for: Therapists with variable caseloads
Practice Management & EHR Solutions
When you need comprehensive mental health practice software that handles everything from scheduling to billing, these established behavioral health EHR platforms offer robust solutions for growing mental health practices.
SimplePractice
SimplePractice all-in-one platform streamlines your entire practice workflow with integrated scheduling, billing, and documentation features for mental health professionals.
- Complete practice management suite with automated appointment reminders
- Built-in telehealth platform with secure client portal access
- Intuitive interface designed for solo practitioners and small group behavioral health practices
- Insurance claims capabilities with claim tracking
Best suited for: Solo therapists and small practices wanting everything in one system
TherapyNotes
TherapyNotes is a comprehensive health EHR solution that excels in clinical documentation while maintaining strong practice management capabilities for behavioral health providers.
- Robust documentation tools with customizable templates and treatment plans
- Advanced insurance claims with electronic submission and tracking
- Established reputation with extensive feature set for clinical workflows
- Strong reporting capabilities for practice analytics
Best suited for: Mental health practices prioritizing detailed clinical documentation and insurance billing
Valant
Valant is enterprise-focused behavioral health EHR scales with larger practices needing advanced functionality. The system supports multiple clinicians across various behavioral health settings.
- Sophisticated reporting and analytics for outcome measurement
- Integrated billing and revenue cycle management
- Advanced compliance tools and audit trails
- Multi-location support with centralized administration
Best suited for: Large group practices and behavioral health organizations
Integration Considerations
Before committing to any health EHR, evaluate how AI documentation tools integrate with your chosen system. Native integrations like Supanote’s “Super Fill” button offer seamless workflows for mental health practitioners, while copy-paste methods require additional tasks.
Specialized Mental Health Platforms
These behavioral health platforms combine EHR functionality with practice management tools while maintaining a focused approach to mental health workflows. They’re ideal for mental health practices seeking comprehensive solutions without the complexity of enterprise systems.
Ensora Health (TheraNest)
Ensora Health offers an affordable all-in-one solution designed specifically for smaller behavioral health practices. The platform combines essential EHR functionality with streamlined practice management tools.
- Budget-friendly pricing structure for solo and small group practices
- Clean, intuitive interface that minimizes learning curve
- Core features include scheduling, billing, and basic documentation
- Simple integrated telehealth for hybrid practice models
Best suited for: Solo practitioners and small practices prioritizing cost-effectiveness over advanced features
ICA Notes
ICA Notes focuses heavily on documentation excellence while providing robust treatment plans capabilities. The platform is built around mental health-specific workflows and compliance requirements.
- Comprehensive treatment planning tools with goal track
- Built-in assessment features and outcome measurement tools
- Strong hipaa compliance support for various mental health regulations
- Templates designed specifically for therapy notes documentation
Best suited for: Mental health professionals who prioritize detailed documentation and treatment planning
Sessions Health
Sessions Health represents the newer generation of behavioral health ehr platforms, emphasizing modern design and automation. The system integrates telehealth seamlessly with practice management.
- Contemporary interface with mobile-friendly design
- Automated appointment reminders and client portal engagement tools
- Integrated telehealth with session recording capabilities
- Regular feature updates and platform improvements
Best suited for: Tech-forward practices wanting modern tools with growth potential
Quick Recap to Mental Health Practice Software
To help you navigate the various options available, here’s a side-by-side comparison of the leading mental health practice software solutions:
AI-Powered Documentation Tools
Tool | Starting Price | Best Suited For |
|---|---|---|
Supanote | $19.99/mo annually (Free plan available) | Built for mental health, native EHR autofill |
Mentalyc | $20/month | Custom workflows, copy-paste to EHR |
Upheal | $19/month (Free tier available) | Built-in telehealth and session analysis |
Blueprint | $29/month | Session-based pricing, recent 2.0 updates |
Practice Management & EHR Solutions
Tool | Starting Price | Best Suited For |
|---|---|---|
SimplePractice | Contact for pricing | All-in-one practice management |
TherapyNotes | Contact for pricing | Comprehensive EHR with billing |
Valant | Contact for pricing | Enterprise behavioral health EHR |
Specialized Mental Health Platforms
Tool | Starting Price | Best Suited For |
|---|---|---|
TheraNest | Contact for pricing | Affordable option for smaller practices |
ICA Notes | Contact for pricing | Documentation-focused with treatment planning |
Sessions Health | Contact for pricing | Modern interface with client engagement |
This comparison highlights the diversity in pricing models and specializations among mental health practice software options, helping you identify which solution aligns best with your practice’s specific needs and budget.
Key Selection Criteria for Mental Health Practice Software
Choosing the right behavioral health ehr software requires careful evaluation of both technical requirements and your specific practice needs.
Essential Evaluation Factors
Start with non-negotiables: HIPAA compliance and robust security standards are mandatory for any system handling client data. Look for encryption, secure data storage, and clear privacy policies.
Consider the learning curve realistically. Even the most feature-rich ehr software won’t help if your team struggles to adopt it.
Test platforms during free trials to gauge actual usability. Evaluate integration capabilities with your existing workflow.
Native EHR system integration saves significant time compared to copy-paste workflows between systems. Analyze total cost of ownership beyond monthly fees.
Factor in training time, setup costs, and potential data migration expenses.
Practice-Specific Needs
Solo mental health practitioners need different features than group practices. Multi-user access, role permissions, and collaborative tools become critical as practices grow.
Specialty-focused behavioral health professionals benefit from platforms offering relevant templates and assessment tools. CBT therapists need different documentation than trauma specialists.
Insurance-heavy practices require robust billing integration with insurance claims processing, while private practice models can prioritize client experience features. Consider scalability early.
Starting with a system that can grow with your practice prevents costly migrations later.
Frequently Asked Questions
Q: What’s the difference between AI documentation tools and comprehensive practice management software?
AI documentation tools focus specifically on generating clinical notes and streamlining documentation for mental health professionals. Practice management software handles scheduling, billing, client portal access, and documentation all in one behavioral health ehr system. Choose AI tools if you’re happy with your current practice management but want better note-taking efficiency.
Q: Can I integrate AI documentation software with my existing ehr system?
Most AI documentation tools integrate with existing behavioral health ehr systems through copy-paste workflows or direct integration. Supanote offers native ehr software integration with a ‘Super Fill’ button, while others like Mentalyc use copy-paste methods. Check compatibility with your specific health ehr before choosing.
Q: How much should mental health practices expect to spend on software monthly?
AI documentation tools typically cost $19-29 per month per provider for mental health professionals. Practice management systems range from $39-89 monthly depending on features. Factor in setup costs, training time, and potential data migration fees when calculating total investment for your private practice.
Q: Is it worth switching from my current mental health practice software to a new system?
Consider switching if your current system significantly slows down your workflow or lacks essential features you need for your behavioral health practice. Evaluate switching costs including data migration, staff training, and temporary productivity loss. Most mental health practices see ROI within 3-6 months if the new system truly fits their needs better.
Q: What security features should I look for in behavioral health ehr software?
Ensure any ehr software you choose has hipaa compliance with end-to-end encryption, secure data storage, and proper access controls for your behavioral health practice. Look for SOC 2 Type II certification and regular security audits. Never compromise on security features to save time when handling sensitive patient information.
Q: How do I know if an AI documentation tool will work with my therapy notes style?
Most AI tools offer free trials or demo periods for mental health practitioners. Test the software with actual patient sessions to see if it captures your therapeutic approach accurately. Look for tools that allow customization of templates and forms to match your preferred documentation style.
Q: Should mental healthcare providers invest in comprehensive practice management software?
Solo practitioners often benefit more from focused solutions rather than comprehensive systems for their private practice. If you already have reliable scheduling and billing processes, an AI documentation tool might provide better value. Comprehensive behavioral health ehr systems work best when you need multiple integrated features to manage your behavioral health practice efficiently.
Q: What happens to my data if I want to switch software platforms?
Most reputable behavioral health providers allow data export, but formats and ease of data migration vary significantly between health ehr systems. Before choosing any ehr software, ask about their data export policies and migration support for your mental health practice. Some platforms charge fees for data migration, so factor this into your decision-making process.
Conclusion
Your ideal mental health practice software depends on your specific workflow, practice size, and priorities for serving patients effectively. Mental health practitioners focused on documentation efficiency often benefit most from AI-powered tools like Supanote to save time on clinical notes.
Behavioral health practices with multiple clinicians typically need comprehensive practice management solutions that integrate scheduling, billing, and client portal features. These systems help therapists focus on patient care while reducing admin tasks and busy work that takes away from treatment.
Take advantage of free trials to test how each behavioral health ehr integrates with your current processes before making your final decision. The right mental health software will help you manage your practice more efficiently, support better patient outcomes, and give you more control over your daily workflow.