Are you spending valuable time writing SOAP notes after patient sessions? As healthcare professionals seek more efficient documentation methods, AI SOAP note generators are transforming clinical documentation.
Let's explore how Supanote's AI SOAP note generator works.
SOAP Notes
Before diving into the technology, let's review what makes effective SOAP notes essential for clinical documentation. SOAP notes consist of four key components:
- Subjective: Patient's symptoms, complaints, and history
- Objective: Observable and measurable findings
- Assessment: Clinical analysis and diagnosis
- Plan: Treatment strategy and next steps
These structured progress notes are crucial for maintaining accurate medical records and ensuring continuity of care.
Evolution from Traditional Note Templates to AI Solutions
Traditional SOAP note templates and shorthand notes have long been used by mental health professionals to save time writing a progress note. While these note templates provide structure, writing progress notes still consumes significant time.
This is where Supanote's SOAP note generator automates the entire documentation process.
Supanote SOAP Note Generator
Supanote offers an advanced AI SOAP note generator that understands your specific session context and can write the different sections of SOAP notes intelligently.
Whether you're documenting individual sessions or developing treatment plans, Supanote can write the note for you. Supanote is specifically focused on mental health notes.
How Supanote's SOAP Note Generator Works
Input Session
Choose your preferred input method:
- Direct session transcribing (with client consent)
- Voice dictation
- You could also upload audio recordings of your sessions if you happen to have them
Automated Note Generation
Within seconds, Supanote creates comprehensive SOAP notes following best practices:
- Scrubs out all personal and protected health information
- Writes a detailed SOAP note with all required sections
- Ensures insurance-ready documentation
Edit/Customize
- Edit the note as needed
- Customize to your own specific style
- Copy-paste the note into your EHR system
It's like having your own AI assistant to do all your documentation, that understands the requirements of clinical documentation.
Let Supanote Write Your Next SOAP Note
Generate structured, HIPAA-compliant SOAP notes in seconds
Try It Free Today!
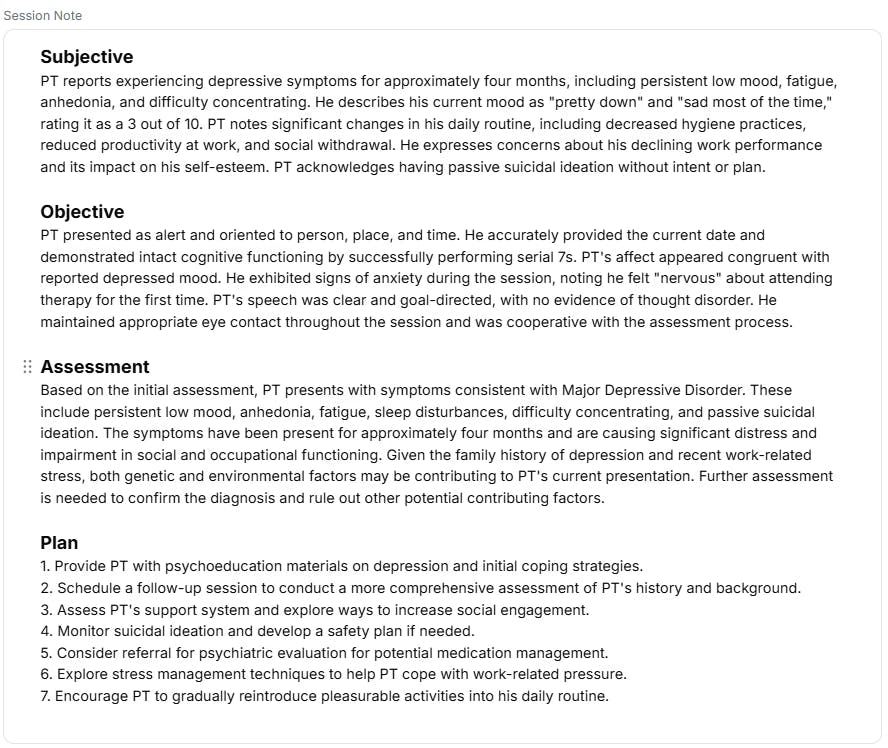
SOAP Note Examples by Supanote
Below is an example SOAP note written by Supanote for a mock therapy session.
Time and Cost Benefits
Time Savings
- Traditional progress note: 5-10 minutes per session
- With Supanote's SOAP note generator: 30-60 seconds
- Documentation time saved each week: 2-4 hours
Cost Analysis
- Free trial with first 10 notes free
- Paid plans start at $20/month
- ROI: Save hundreds of hours each year
Security and Professional Standards
Supanote prioritizes the security of your clinical documentation:
- Supanote is fully HIPAA compliant
- No audio recording of sessions is ever stored
- All PHI/PII information is automatically scrubbed
- Data is fully encrypted in transit and at rest
- Professional best practices for data handling
Get Started with Supanote in <1 minute
- Try the product for free (no credit card required)
- Get your first SOAP note
- Begin streamlining your documentation process
How does an AI Note generator work?
AI Scribes or Ai note generators might seem like magic, but here's a simplified version of what happens:
- Recording: The literal audio waves from your conversation are captured.
- Convert to Text/Transcription: The captured audio is converted to text. This technology is highly accurate (99%+) now and can account for a variety of accents and styles of talking.
- Understand the context: This is the AI part. The AI analyzes the text to understand its meaning. It identifies key themes, emotions, and clinical relevance. They use natural language processing (NLP) to do this.
- Write clinical session note: Here's where the AI scribe writes the note using the structured format- it uses what it's learned from thousands of therapy sessions to write a coherent note.
The key here is that the AI isn't just transcribing. It's understanding and summarizing. It knows that when a client says "I've been feeling really down lately," that's likely to go in the "Subjective" part of a SOAP note. Which is why these tools feel magical to anyone who uses it for the first time. Read this article for a comprehensive overview of how these tools work.
AI therapy Notes vs AI medical scribe
There are two kinds of tools in the market:
1. Therapy Note tools built specifically for psychologists/therapists/mental health
2. Generic AI medical scribes write medical notes for all medical professionals like physicians, physical therapists etc.
If you're a therapist, the former product will make more sense for a couple of reasons. Why?
One, the quality of the note is usually better because it's custom-built for psychologists. For example, Supanote is trained with 1000s of real-life insurance-approved session notes.
Second, the range of notes an AI Therapy Note tool can write are broader than generic AI medical scribes which tend to do just SOAP notes. You can compare the top therapy note tools here.
FAQs About SOAP Note Generator
Q: How does Supanote compare to traditional note templates?
A: Supanote's SOAP note generator creates comprehensive clinical notes in seconds. It typically provides more detailed documentation than traditional templates to ensure insurance-readiness. You can adjust the level of detail to suit your preference.
Q: Can I customize the SOAP note templates?
A: Yes, you can customize all note templates to match your specific needs and practice requirements.
Q: How secure is the clinical documentation process?
A: Supanote maintains HIPAA compliance and employs enterprise-grade security for all clinical notes.
Q: Can I use this for other types of progress notes?
A: Yes, Supanote supports multiple note formats, including DAP notes, BIRP, GIRP, PIE, and many more. It can also write couples and group therapy notes.
Q: What if I need to modify my treatment plans?
A: The platform allows easy updating of treatment plans and clinical documentation.
Q: Does it work for different medical specialties?
A: Yes, Supanote automatically adapts its note-writing style based on your medical specialty and practice type.
Transform Your Clinical Documentation Today
Supanote's SOAP note generator offers healthcare professionals a powerful tool to streamline their documentation process while maintaining high-quality clinical notes. Whether you're writing progress notes, developing treatment plans, or managing other aspects of clinical documentation, Supanote helps you focus more on patient care and less on paperwork.
Visit Supanote.ai today to start your free trial and experience the future of clinical documentation. You can also compare and contrast different AI documentation tools here.
Save 4 Hours Every Week on SOAP Notes
Supanote auto-generates SOAP notes in under a minute so you can get back to doing what matters - seeing clients
Get Started for Free Today!