We've all had those sessions where something feels distinctly off.
The patient who's typically sharp and engaged now struggles to follow the conversation. The usually well-groomed client arrives disheveled and disoriented. The calm, composed individual suddenly exhibits agitation and confusion.
And that nagging clinical intuition tells you: this is an altered mental status – a change in their cognitive functions that requires your immediate attention. But when it comes time to document and code these presentations, many mental health professionals feel unsure.
Which ICD-10 code for altered mental status accurately captures what we're observing?
Is R41.82 (unspecified altered mental status) appropriate, or should we use a more specific code?
What documentation best supports our clinical judgment while ensuring accurate diagnosis and proper reimbursement?
For all these questions, this guide breaks down the essentials of altered mental status ICD-10 coding for mental healthcare providers, with practical approaches you can implement immediately to improve patient outcomes.
What Exactly Is "Altered Mental Status"?
Altered mental status (AMS) is a broad term referring to signs involving cognitive functions, including disorientation, changes in cognition, behavior, or awareness.
Unlike specific mental health conditions such as depression or anxiety, AMS is a symptom rather than a definitive diagnosis - a clinical presentation that stems from various underlying factors requiring thorough assessment. Conditions like delirium, dementia, encephalopathy, psychiatric conditions, and substance intoxication or withdrawal can all lead to altered mental states.
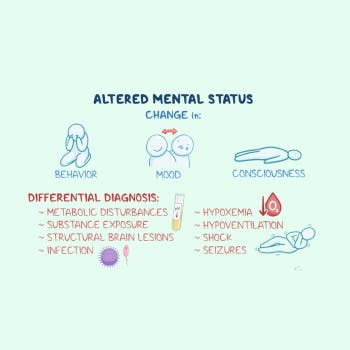
AMS exists on a spectrum ranging from mild confusion to a severely altered level of consciousness. Certain groups, including older adults and those with neurological conditions, are at higher risk for altered mental status:
- Mild: Subtle changes in attention, concentration, processing speed, or emotional state
- Moderate: Clear disorientation, confusion, agitation, cognitive deficits, or unusual behavior
- Severe: Marked impairment in consciousness (often measured by the Glasgow Coma Scale), unresponsiveness, or inability to communicate coherently
As mental health professionals, recognizing these variations is crucial for accurate coding, differential diagnosis, and developing comprehensive care plans. Altered mental status can affect patients of all ages, including children, though the symptoms can differ.
Essential ICD-10 Codes for Altered Mental Status
The ICD-10-CM system offers several specific codes that capture altered mental status presentations. Accurately coding these signs involving cognition helps ensure proper treatment and reimbursement. R41.82 is considered by payers to be a billable code for reimbursement purposes.
R41.0 - Disorientation, Unspecified
This code applies when a patient demonstrates confusion about time, place, or person without a clearly identified underlying cause. Use this code when:
- The patient exhibits general confusion in mental state
- There's disorientation to time, place, or person
- The condition appears acute rather than chronic
- The underlying medical conditions remain unidentified despite clinical assessment
Clinical Example: A 45-year-old patient with no previous cognitive issues or recent head injury suddenly has difficulty recognizing family members and is confused about current dates and locations, requiring further evaluation.
R41.82 - Altered Mental Status, Unspecified
This is the most general code for altered mental status (mental status unspecified R41.82) and should be used when:
- Changes in mental status don't fit more specific categories or other symptoms
- The presentation includes vague or mixed signs involving cognitive functions
- You're still working toward identifying factors contributing to the patient's altered mental status
- Laboratory tests and comprehensive evaluation haven't yet revealed the underlying cause
Clinical Example: A typically high-functioning patient presents with new-onset confusion, slowed responses, and difficulty following simple instructions, necessitating both psychiatric and neurological assessment.
F05 - Delirium Due to Known Physiological Condition
When altered mental status presents as delirium with an identified physiological condition:
- Disturbed attention and awareness with cognitive deficits
- Additional cognitive disturbances (memory deficit, disorientation, language disturbance)
- Develops over a short period and fluctuates throughout the day
- Evidence suggests metabolic imbalances, electrolyte imbalances, or hepatic failure
Note: This code requires a second code to identify the specific physiological condition, as delirium NOS requires further information.
Clinical Example: An elderly patient showing confusion and agitation due to substance intoxication or UTI-induced delirium, requiring a specific diagnosis beyond the broad term of altered mental.
F44.89 - Other Dissociative and Conversion Disorders
When altered mental status appears to result from psychological stressors rather than medical conditions:
- Sudden onset of cognitive changes following emotional stress
- No identifiable neurological disorders or other medical cause
- May appear after traumatic brain injury or relate to mental disorders
- Symptoms may include confusion, disorientation, or memory disturbances
Clinical Example: A patient experiencing dissociative symptoms following severe trauma, resulting in an altered mental state regarding identity and personal history, warranting a specific code rather than an unspecified mental disorder classification.
Managing Altered Mental Status: From Assessment to Accurate Coding
Proper coding requires a thorough assessment and detailed documentation. While comprehensive medical evaluation often occurs outside our scope of practice, mental health professionals play a crucial role in the initial detection and referral process. Determining the underlying cause of altered mental status requires a thorough assessment including medical history, physical examination, laboratory tests, and imaging studies.
1. Mental Status Examination Components
Document these key elements when the patient presents with altered cognition:
- Appearance: Grooming, posture, unusual movements
- Behavior: Agitation, restlessness, unusual mannerisms
- Mood/Affect: Emotional state, appropriateness to situation
- Speech: Rate, volume, coherence, content
- Thought Process: Logic, organization, associations
- Thought Content: Delusions, obsessions, suicidality
- Cognition: Orientation, memory, attention, calculation
- Insight/Judgment: Understanding of condition, decision-making capacity
Consider using brief screening tools like the Mini-Mental State Exam (MMSE), MoCA, or Glasgow Coma Scale to quantify changes and support your clinical documentation, especially when referring for medical evaluation.
2. Exploring Psychiatric Conditions
Consider whether the presentation might better align with specific psychiatric conditions:
- Major depressive disorder with cognitive impairment
- Acute psychosis or unspecified mental disorder
- Dissociative disorders related to trauma
- Substance use disorders or substance intoxication
- Anxiety-related depersonalization/derealization
- Neurocognitive disorder requiring a specific diagnosis
3. Screening for Medical Red Flags
Watch for concerning signs that warrant immediate medical attention to identify underlying medical conditions:
- Sudden onset of severe symptoms suggesting an altered level of consciousness
- Accompanying physical symptoms (headache, fever, etc.)
- Recent medication changes, substance use, or recent illnesses
- History of traumatic brain injury or other neurological disorders
- Metabolic imbalances that might be detected through laboratory tests
Documentation Best Practices for Accurately Coding Altered Mental Status
Your thorough documentation not only supports patient care but also justifies your coding choices to third-party payers. For altered mental status presentations, ensure your documentation includes:
1. Baseline Comparison
Always note how the patient's condition differs from their baseline mental state:
"Patient typically demonstrates coherent thought processes and full orientation but today exhibited tangential thinking and confusion about the current date and recent events, suggesting an altered mental state requiring further evaluation."
2. Objective Behavioral Observations
Document specific behaviors rather than general impressions to support the correct code:
"Patient required questions to be repeated multiple times, lost track of conversation mid-sentence, and referred to the therapist by an incorrect name. These signs involving cognitive functions suggest potential unspecified altered mental status (R41.82)."
3. Comprehensive Mental Status Examination
Include detailed observations across all MSE domains for thorough documentation:
"Orientation: Oriented to person, disoriented to place and time. Attention: Unable to complete serial 7s or spell 'world' backward. Memory: Impaired recall of recent events but intact remote memories. Thought process: Tangential with occasional word-finding difficulties, suggesting cognitive deficits requiring the 10 code for altered mental status."
4. Diagnostic Reasoning
Explain your clinical decision-making regarding potential underlying factors:
"Given the gradual onset, absence of physical symptoms, and correlation with increased life stressors, patient's altered mental status appears more consistent with dissociative symptoms than an underlying medical condition. However, differential diagnosis including neurological disorders is warranted."
5. Intervention and Safety Plan
Detail your response to ensure comprehensive care when managing altered mental status:
"Recommended immediate medical evaluation to rule out metabolic imbalances or other physiological condition. Provided crisis resources and arranged follow-up within 24 hours. Contacted emergency contact (with patient permission) to ensure safe transport for further evaluation of the patient's condition."
Differential Coding Scenarios
Scenario 1: AMS with Unknown Cause
- 73-year-old patient with sudden confusion, no obvious medical issues
- Primary Code: R41.82 (Altered mental status, unspecified)
- Documentation Focus: Detailed mental status exam, baseline comparison, medical referral
Scenario 2: AMS with Suspected Medical Cause
- 52-year-old with new-onset confusion and known diabetes
- Primary Code: R41.82 (Altered mental status, unspecified)
- Secondary Code: Consider Z79.4 (Long-term insulin use) to note risk factor
- Documentation Focus: Specific symptoms, medical history, urgent referral
Scenario 3: AMS Related to Psychiatric Condition
- 29-year-old with confusion during acute panic attack
- Primary Code: F41.0 (Panic disorder)
- Secondary Code: Not necessary unless the altered mental status persists beyond the expected panic symptoms
- Documentation Focus: Relationship between panic symptoms and cognitive changes
Scenario 4: Post-Traumatic Dissociative Symptoms
- 35-year-old trauma survivor with episodic disorientation and identity confusion
- Primary Code: F44.89 (Other dissociative and conversion disorders)
- Documentation Focus: Trauma history, relationship between trauma triggers and symptoms, differentiation from organic causes
Automating Therapy Documentation with AI
With the rise of AI-powered tools, mental health professionals are increasingly turning to AI Therapy Note tools like Supanote to streamline documentation—especially in complex cases involving altered mental status ICD-10 coding. These tools can:
- Automatically create nuanced clinical documentation that captures signs involving cognitive functions
- Can automatically identify the appropriate ICD-10 code for altered mental status based on your session notes
- Prevent billing and coding errors when using specific codes versus unspecified code options
- Reduce time spent on paperwork, allowing more focus on patient care and improving patient outcomes
For example, at the end of a session involving altered mental status assessment, Supanote would directly generate the relevant progress notes in your preferred format (SOAP, DAP, GIRP, etc.), along with a detailed mental status examination, and suggest whether mental status unspecified R41.82 or a more specific diagnosis code like F05 (delirium due to known physiological condition) would be appropriate based on your clinical observations.
Ready to try? 10 notes on us!
Login to your Supanote account and instantly access 10 free notes
Get It Now!
Risk Management for AMS Cases
Altered mental status presentations carry significant clinical and legal risks:
1. Liability Considerations
- Document all referral recommendations and the patient's response
- Note any refusals of recommended medical evaluation
- Record all attempts to ensure patient safety
- Consider capacity issues in treatment planning and informed consent
2. Informed Consent Adaptations
- Assess capacity to consent to psychological treatment
- Consider temporary substituted consent from authorized representatives when appropriate
- Document capacity assessment process clearly
- Revisit consent when mental status improves
3. Safety Planning
- Develop specific protocols for AMS emergencies in your practice
- Create documentation templates that prompt thorough assessment
- Maintain current referral relationships with medical providers
- Establish clear follow-up procedures for post-medical evaluation
Case Example: Putting It All Together
Initial Presentation: 58-year-old female presents with sudden confusion during session, difficulty remembering recent events, and mild word-finding problems. Medical history includes recent sleep changes but no known neurological disorders or recent head injury.
Assessment Actions:
- Conducted thorough mental status exam showing disorientation to date and mild cognitive deficits
- Contacted emergency contact (with patient permission) to gather further information about patient's altered mental status
- Learned about recent medication change and substance use from family member
- Referred for comprehensive evaluation due to concerns about an underlying condition
Documentation:
- Used R41.82 (Altered mental status, unspecified) as preliminary code, noting this is a broad term requiring further specificity
- Detailed specific changes in cognitive functions from baseline mental state
- Documented referral recommendations to rule out factors contributing to altered mental
- Noted plan for follow-up after laboratory tests and medical evaluation
Outcome:
- Medical evaluation revealed adverse medication reaction and electrolyte imbalances
- Updated from the unspecified code to F05 (Delirium due to known physiological condition) with T50.905A (Adverse effect of unspecified drugs) as the specific code
- Modified treatment plan to address psychological impact of the physiological condition
- Coordinated with other healthcare professionals on ongoing monitoring of the patient's condition
FAQs about Altered Mental Status ICD-10
Q: Can I use altered mental status ICD 10 code (R41.82) as a primary diagnosis for ongoing therapy?
A:No. R41.82 shouldn’t be used as a primary diagnosis for ongoing therapy. It’s valid for short-term use when the cause of the altered mental status is unclear, but since R-codes represent symptoms not diagnoses clinicians should update the code once the underlying mental, medical, or neurological condition is identified.
Q: If a patient presents with altered mental status but refuses medical evaluation, what should I do?
A: Document your recommendation for thorough assessment, the patient's refusal, and your evaluation of their decision-making capacity. If safety concerns are significant due to the patient's altered mental state, consider emergency protocols according to your state laws regarding duty to protect.
Q: How detailed should the mental status examination be to support accurate coding of altered mental status?
A: Your MSE should include specific observations across all domains with detailed documentation of cognitive deficits. Quantitative measures using the Glasgow Coma Scale or other standardized assessments provide stronger support for the mental status ICD 10 code than qualitative statements about mental state.
Q: Can I bill for extended sessions when a patient unexpectedly develops signs involving cognitive functions?
A: Yes, with thorough documentation. Use the appropriate CPT code for extended sessions such as 90837 (60-minute psychotherapy) or 90839/90840 (crisis intervention) and clearly document how managing altered mental status required additional assessment time, safety planning, and coordination with healthcare professionals for comprehensive care.
Q: How do I code when altered mental status resolves during my assessment?
A: If symptoms completely resolve and a specific diagnosis is identified (e.g., substance intoxication, psychiatric conditions), code the underlying condition. If the episode resolves but factors contributing remain unclear, you can still use unspecified altered mental status (R41.82) while documenting the temporary nature of the symptoms.
Q: Should I use altered mental status codes for cognitive symptoms in mental disorders like ADHD or depression?
A: No. When cognitive deficits are characteristic features of a psychiatric diagnosis (e.g., concentration difficulties in ADHD or depression), code the specific mental health condition rather than using separate codes for signs involving cognitive functions.
Have Your AMS Notes Written for You
Document AMS, generate ICD-10, effortlessly with Supanote
Get It Now!
Additional Resources for Mental Health Professionals
- Understanding Cognitive Assessment for Altered Mental Status
- Medical Emergencies in Psychotherapy: Managing Altered Mental Status
- Documentation Best Practices for Mental Health Conditions
- ICD-10 Code for Altered Mental: Updates for Mental Healthcare Providers
- Traumatic Brain Injury and Altered Mental Status: Assessment Guidelines
By developing expertise in recognizing, documenting, and appropriately coding altered mental status ICD 10, you strengthen your clinical practice while ensuring proper reimbursement and optimal patient outcomes. Remember that these presentations often represent critical moments in patient care where your assessment skills and professional judgment make a significant difference.
When in doubt about a patient's altered mental state, err on the side of caution with prompt referral for further evaluation and maintain detailed documentation throughout. Your thorough notes not only support accurate coding but ultimately serve your patients by ensuring comprehensive care during vulnerable moments.