Daily documentation is one of the most time-consuming- and honestly, most stressful- parts of an SLP’s workload.
Between back-to-back sessions, managing IEPs, and coordinating with families and staff, it’s easy for notes to pile up or become inconsistent.
That’s when a well-structured speech therapy daily notes template can save the day.
Now, while there are several note formats therapists can use to document, like SOAP, BIRP, or DAP, we’ll be focusing on the SOAP format in this guide as it’s one of the most widely used across schools, clinics, and private practices.
A streamlined SOAP note template can help you:
- Save time between sessions
- Maintain clarity and compliance
- Track client progress effectively
- Reduce the cognitive load of daily paperwork during therapy sessions
In this guide, you’ll discover exactly what to include in your therapy notes to meet clinical, legal, and professional standards.
Let’s dive into how to create and use a customizable SOAP note template that works for your caseload and not against it.
Why Daily Notes Matter in Speech Therapy
Writing daily SOAP notes isn’t just a routine task; it plays a key role in quality care, billing, and communication. Here’s why they matter:
- Supports Clinical Work
SOAP note documentation shows what you did during the session and why it matters for the client’s progress. - Protects Your License
Clear daily notes show your clinical decisions and support professional accountability. - Meets Legal and Billing Rules
Your speech therapy session notes must follow state, payer, and federal documentation rules to avoid billing issues or audit problems. - Follows ASHA and HIPAA Guidelines
Well-written SOAP notes help you stay in line with ASHA’s and HIPAA’s standards, especially when using EMRs. - Tracks Progress Clearly
Using the SOAP format lets you monitor how the client is doing with their therapy goals, week by week. - Helps Team Communication
Strong documentation helps coordinate with families, occupational therapists, teachers, and others involved in the client’s care. - Maintains Professional Standards
Good note writing builds trust in your work. Well-organized session notes help other speech therapists understand and continue your work if needed. - Shows Clinical Reasoning
A solid SOAP note example with objective data and clear strategies helps explain your decisions. - Improves Documentation Quality
A consistent speech therapy daily notes template makes it easier to record outcomes, data, and therapy goals accurately. - Supports Continuity Across Settings
Whether you're documenting individual sessions or managing private practice clients, strong SOAP note documentation ensures clear communication and accurate documentation.
What to Include in a Daily Notes Template
A reliable speech therapy daily notes template is built to capture every therapy session’s essence.
Your template form should be standardised, yet flexible enough for tailored notes.
Core Details to Include in Every Daily Note
Start with the foundational elements:
- Date and time of session
Important for accurate timelines and billing audits. - Type and duration of service
Clarify whether it was in-person, group, teletherapy, etc. - Client identifiers
Use initials or codes to remain HIPAA-compliant while keeping entries clear. - Current goals
Should align with IEPs or treatment plans (e.g., “increase accuracy of /r/ in connected speech”). - Objective data
Example: “Client achieved 70% accuracy producing /r/ over 15 trials.” - Subjective observations
Note mood, attention span, engagement, or behavior impacting performance.
Using the SOAP Format
Many SLPs prefer the SOAP format for its structure and clarity. Here’s how each section works:
- S (Subjective): What the client or caregiver shares
E.g.,“Client reported difficulty using AAC at home.” - O (Objective): Measurable, data-driven results
E.g.,“Produced /s/ with 80% accuracy during word-level drills.” - A (Assessment): Your clinical interpretation
E.g.,“Increased independence with cueing; progress consistent with IEP goals.” - P (Plan): Next steps
E.g.,“Introduce minimal pairs and continue targeting initial /s/ in connected speech.”
Optional But Valuable Add-Ons
To paint a fuller picture of the session, consider including:
- Materials/activities used
E.g., “barrier games, digital visuals, flashcards.” - Specific interventions
E.g., “Used visual cues and tactile prompts for accuracy.” - Breakthroughs or barriers
E.g., “Client independently corrected /s/ without prompting.” - Caregiver input
E.g., “Parent noted increased use of sign language during dinner.”
Tip: Adding checklists or dropdowns for these fields can make note-taking faster and more consistent.
Using customizable check boxes for progress markers or strategies used can make writing notes much faster. This method not only helps with clear session documentation but also makes things easier to review during audits.
Here’s a simple example of a printable daily notes template that many SLPs use to stay consistent across sessions:
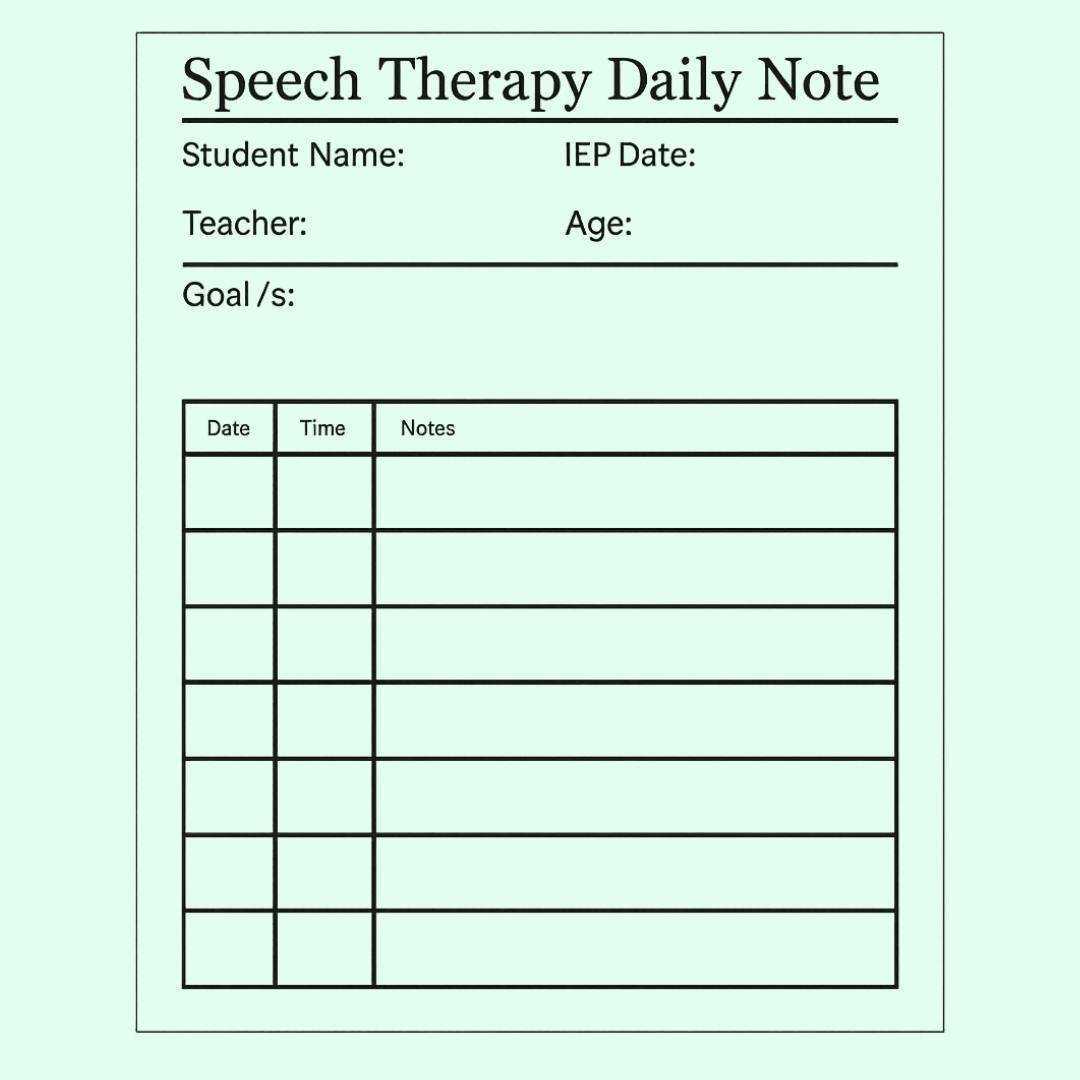
A well-structured therapy note form helps you stay focused on client care. When the format matches how you conduct therapy sessions, your SOAP note clearly shows what happened and why it matters.
Speech Therapy Daily Notes Template Examples
Here are a few example entries using the SOAP format across different speech therapy contexts:
Articulation Therapy (School Setting)
S: Client stated they were excited to work on /s/ sounds today.
O: Client achieved 80% accuracy producing /s/ in initial position during structured activities (16/20 trials).
A: Demonstrates improvement with visual cueing; progress consistent with IEP goals.
P: Continue targeting /s/ in mixed word positions; introduce minimal pair activities.
Language Therapy (Private Practice)
S: Parent reported client is using more complex sentences at home.
O: Client produced 4+ word utterances with 75% accuracy during narrative retell tasks.
A: Increased sentence complexity and reduced prompt dependence; gains aligned with treatment plan.
P: Introduce story generation tasks; model descriptive language using picture books.
AAC User (Teletherapy)
S: Caregiver shared concerns about limited engagement with the device at school.
O: Client used AAC to initiate communication in 5 out of 7 structured opportunities.
A: Emerging use of AAC for functional requests; requires modeling and aided language input.
P: Increase modeling of core words in routines; collaborate with the classroom team.
Save Hours on Speech Therapy Documentation
Supanote auto-generates SOAP notes from your speech therapy sessions
Start your Free Trial Today!
Templates That Work: Examples & Tools
Using the right speech therapy daily notes template can help you avoid burnout, improve accurate documentation, and make it easier to communicate effectively with other service providers.
No matter where you work- private practice, school, or hospital- the tools you choose matter.
1. Handwritten Templates
For speech therapists who prefer writing by hand, printed templates are a great option:
- Great for low-tech setups or those who prefer handwriting
- Keep a binder with checklists based on therapy goals
- Add sections for client behavior and caregiver notes
Tip: Scan or store notes in a secure, HIPAA-compliant cloud after sessions
2. Editable Documents (Word/Google Docs)
Great for both schools and private practice:
- Works well for speech therapy session documentation
- You can also add dropdowns for common objectives and cues
- Helps with SOAP note formatting while staying editable
These templates let you reuse notes weekly and tweak them for each client’s needs.
3. SLP-Tailored Templates by Therapy Focus
Use different templates based on diagnosis to target therapy goals better:
- Articulation: sound cues, placement, errors
- Language Disorders: syntax, narrative, pragmatics
- AAC Users: button use, home practice, parent input
Organize your SOAP note example library by client age, diagnosis, and therapy type.
Build once, reuse often.
Pro Tip: Add reusable phrases to your SLP SOAP templates to speed up note writing.
Your SOAP note template should support your practice, save time on note-taking, and keep your accurate documentation strong over time.
How to Make Daily Documentation Faster and Easier
Documentation efficiency comes from repeatable writing strategies:
1. Phrase Banks
Save reusable phrases like “client produced target sound with 85% accuracy in structured tasks” and paste them into session notes.
2. Smart Abbreviations
Use abbreviations like “VPM” (Visual Phonemic Model), “MVF” (Minimal Verbal Feedback) include a key in your slp soap protocol.
3. Copy & Tweak Therapy Goals
Reusing well-written therapy goal banks and editing per session outcome always helps in streamlining things
4. Batch Note Completion
Try reserving 20 minutes midday or afternoon to complete SOAP notes for five therapy sessions. It keeps data fresh.
5. Voice Dictation
Use secure tools like Microsoft Dictate, Supanote, or EMR voice entry to speak your SOAP note example as if explaining to another SLP.
6. Pre-Filled Templates
Set therapy notes by preloading current plan notes, treatment plans, and cues used.
By streamlining your SLP soap process, you save time while ensuring your documentation remains complete and defensible.
Common Mistakes (and How to Avoid Them)
Even an excellent SOAP note template doesn’t inoculate against missteps. Here’s what to avoid:
1. Over- or Underdocumenting
Watch note length, avoid overly narrative therapy notes. Be concise, referencing goals and client’s behavior when needed.
2. Switching Terminology Midweek
Ensure consistency in how you describe objectives and supports. Use the same terminology in SOAP notes week after week.
3. Breaching Privacy Compliance
Never include the client’s full name, date of birth, or PHI in shared platforms unless secured. Store documents only in encrypted, HIPAA-compliant systems.
Using a standardized SLP SOAP note not only guards against these pitfalls, but it also improves professional communication and supports future sessions.
Skip the Mistakes, Automate Your Notes
Supanote helps SLPs generate accurate, ready-to-bill SOAP notes with the least effort
Start your Free Trial Today!
Building Your Own Speech Therapy Notes Template
Customizing your SOAP note template allows you to:
- Build accurate documentation
- Align SOAP notes to daily clinical practice
- Collect relevant data across therapy sessions
Start by designing forms suited to your context:
- School-Based Templates: Track IEP status, include teacher collaboration checkboxes.
- Private Practice Templates: Include CPT billing codes, session billing types, therapy room location, and family notes.
- Teletherapy Templates: Add internet connection notes, platform used, and client engagement metrics.
Also,
- Include structured fields for the subjective section, the objective section, and assessment section.
- Maintain a logical treatment plan progression between SOAP note logs.
- Keep the design simple and repeatable with check boxes and dropdowns to save time.
Before wide adoption, test your SLP SOAP note template across various clients - articulation, language, AAC. Add improvements based on real-time case data usage.
Frequently Asked Questions
Q. What is a speech therapy daily notes template?
A. It’s a structured format—usually based on the SOAP method—that helps SLPs document sessions clearly and consistently.
Q. Why should I use a daily notes template for speech therapy?
A. Templates save time, ensure you meet compliance standards, and make it easier to track client progress over time.
Q. What’s included in a strong speech therapy SOAP note?
A. The template should include fields for subjective input, measurable objectives, clinical assessment, and a plan for the next session.
Q. Can I use the same template for school and private practice?
A. Yes, with minor tweaks. A good template should be flexible enough to adapt to IEP tracking, insurance billing, and session goals.
Q. How do templates help with documentation accuracy?
A. Templates reduce missed details, support clinical reasoning, and make it easier to stay consistent across sessions and clients.
Q. What are some optional fields to include?
A. You can add checkboxes for cueing strategies, session materials, caregiver feedback, and client behavior for richer documentation.
Q. How do I customize a SOAP note template for different client needs?
A. Segment templates by age, diagnosis (e.g., articulation, AAC), or setting (teletherapy vs in-person) to make documentation smoother.
Q. Are there free tools or platforms to help with daily notes?
A. Yes, tools like Supanote offer pre-built, editable SOAP templates that can be auto-filled or customized for faster note writing.
Q. How often should I update or revise my template?
A. Whenever your caseload changes, you introduce new therapy goals, or billing requirements are updated.
Q. How does Supanote make SOAP note templates easier to use?
A. Supanote auto-generates SOAP notes from your input (text or audio) and allows for customization—so your notes are fast, accurate, and client-specific.
Free Resources and Where to Find Quality Templates
Finding the right SOAP note template doesn’t require reinventing the wheel.
Here are free resources that are famous among speech-language pathologists:
- Supanote: Offers SLP-designed tools tailored for SOAP documentation efficiency.
- Teachers Pay Teachers (TPT): Thousands of downloadable, customizable therapy note templates by speech therapists.
- Facebook Groups & SLP Blogs: Great for peer-reviewed examples, shared download links, and template ideas.
Evaluate each form to check:
- Is it HIPAA compliant?
- Is it easy to customize to match your client population or private practice needs?
- Does it support billing standards?
Using templates and SOAP note examples from trusted communities lets you focus more on sessions, less on writing notes.
Conclusion
Strong SOAP documentation practices help improve client care, support clinical decisions, and build your professional credibility.
Whether you’re working in group therapy or individual sessions, being able to clearly document data, behavior, and progress during therapy sessions can impact your client’s outcomes.
Using the right SLP SOAP note template can help streamline your day.
Whether it’s handwritten, digital, or built using tools like Supanote, the best SOAP note template is one you’ll actually stick with.
Remember:
- Include a subjective section, an objective section, assessment notes, and a clear plan section
- Use editable templates with check boxes to save time during data entry
- Make sure your notes clearly show the client’s treatment and progress over time
Your SOAP note is more than just a document- it's your professional voice.
Therefore, each entry should communicate effectively what you did, why it matters, and what’s next.