This guide breaks down everything you need to know about the 90792 CPT code - from documentation requirements to maximizing reimbursement rates - so you can focus on what matters most: providing excellent care to your mental health clients.
What Is the 90792 CPT Code?
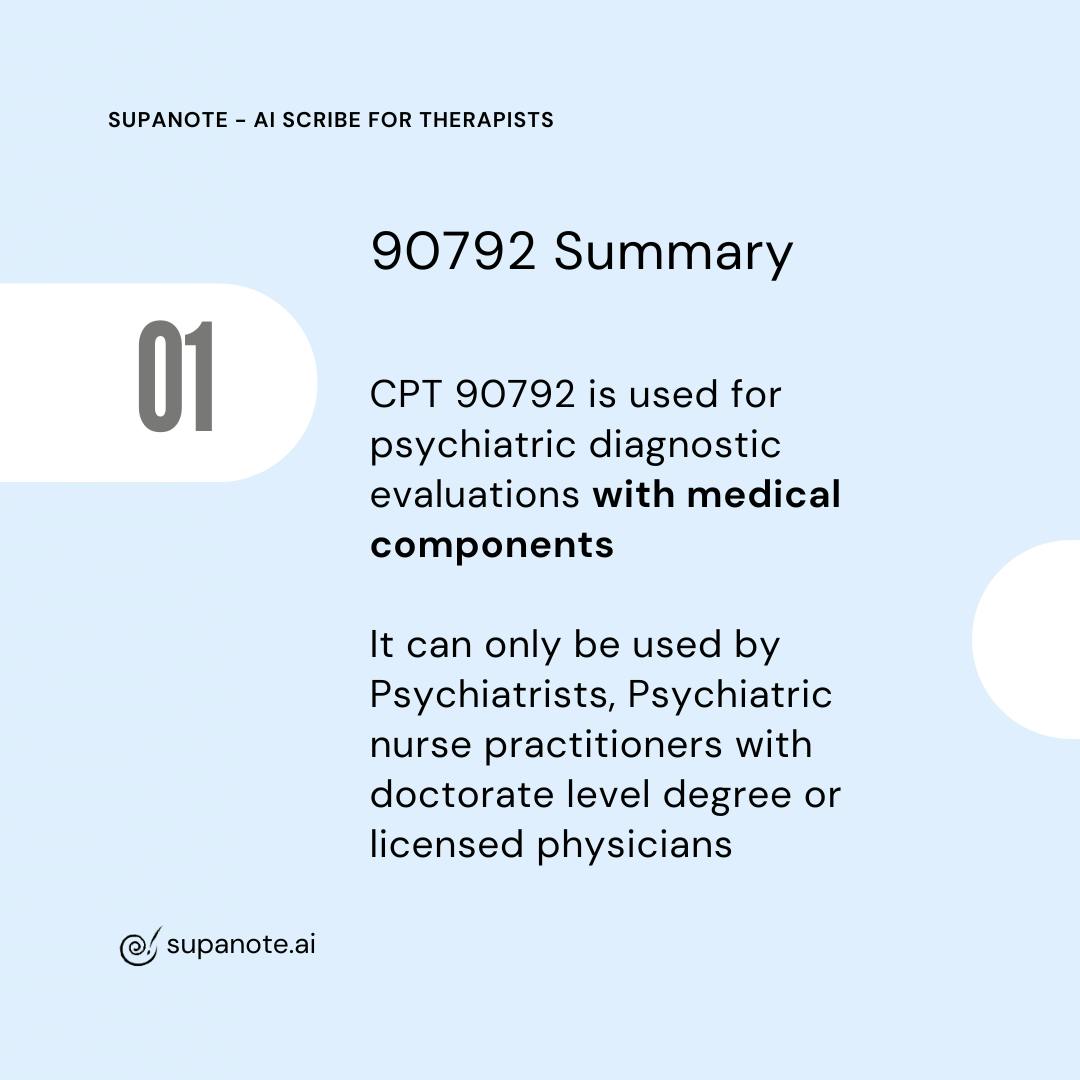
The 90792 CPT code represents a "Psychiatric diagnostic evaluation with medical services" also known as a psychiatric diagnosis interview examination.
This code, established by the American Medical Association, covers an exhaustive diagnostic interview that includes both:
- Psychiatric assessment, and
- Medical assessment components
Unlike its counterpart 90791 (psychiatric diagnostic evaluation without medical components), 90792 specifically includes evaluation and management services performed by qualified healthcare professionals who can provide medical services as part of the initial diagnosis evaluation.
Who Can Use the 90792 CPT Code?
The 90792 CPT code is restricted to licensed medical professionals who can deliver medical services:
- Psychiatrists (medical doctor/MD/DO)
- Psychiatric nurse practitioners
- Licensed physician or physician assistants working in psychiatry
Note: Clinical psychologists, licensed clinical social workers, and marriage and family therapists typically cannot bill using 90792 as they aren't authorized to provide the physical exam component and other medical services. These behavioral health providers should use 90791 instead for the diagnostic interview.
Key Components of a 90792 Evaluation
A comprehensive psychiatric diagnostic evaluation with medical components must include these elements:
- Complete psychiatric history
- Mental status examination establishment
- Medical components, which may include:
- Vital signs assessment
- Physical exam component
- Complete medical history review
- Medication management considerations
- Management service performed
- Patient's ability assessment
- Initial diagnosis of mental disorders
- Initial treatment plan development
The medical assessment components are what distinguish CPT code 90792 from other mental health services and justify the higher reimbursement rates that Medicare and Medicaid programs provide to psychiatrists and other qualified providers.
Billing Considerations for 90792
Time Spent Requirements
The 90792 code doesn't specify a minimum time requirement. However, the intake session depend on complexity and typically takes 60-90 minutes to complete thoroughly. Always document the actual time spent with the mental health clients.
Frequency Limitations
Most insurance companies limit psychiatric diagnostic evaluations (both 90791 and 90792) to one per year per same provider, though exceptions exist for:
- Significant changes in clinical status
- New episodes after resolution of previous conditions
- Evaluations by different specialists
Benefits verification should be completed before services provided, as providers require different documentation.
Reimbursement Rates
Reimbursement rates for 90792 are typically 20-30% higher than 90791 due to the medical services involved. Average reimbursement varies depending on several factors:
- Geographic location
- Insurance billing policies
- Provider credentials
- Medicare Medicaid guidelines
- Contract negotiations
Recent Medicare Rates for 90792:
- 2025: $185.18
- 2024: $190.57
- 2023: $196.55
- 2022: $218.90
- 2021: $201.68
Documentation Requirements for 90792
Your documentation for performing services under 90792 should clearly demonstrate the medical services that justify using this procedure code for a comprehensive psychiatric evaluation. Don't forget to include:
- Patient identification information
- Chief complaint and psychiatric history
- Medical history with necessary detail
- Current medications and pharmacologic management considerations
- Substance use history
- Family psychiatric and medical history
- Mental status examination establishment
- Physical exam component findings (crucial for 90792)
- Medical necessity documentation
- Risk assessment
- Psychiatric diagnosis (or differential diagnosis)
- Treatment plan recommendations
- Time spent with the client
Have your progress notes written for you for free!
Try Now!
Sample Session Note for CPT Code 90792
Below is a comprehensive example of a properly documented psychiatric diagnosis interview examination using cpt code 90792:
PSYCHIATRIC DIAGNOSTIC EVALUATION WITH MEDICAL SERVICES (CPT CODE 90792)
Date of Service: 4/26/2025
Start time: 10:15 AM - End time: 11:45 AM
Total time spent with patient: 90 minutes
PATIENT IDENTIFICATION INFORMATION:
Jane Doe, DOB: 05/15/1985, MRN: 12345678
CHIEF COMPLAINT: "I've been feeling depressed and anxious for months now, and I can't seem to sleep. I'm worried about my blood pressure too."
PSYCHIATRIC HISTORY:
Patient reports onset of depressive symptoms approximately 4 months ago, coinciding with job loss. Symptoms include persistent low mood, anhedonia, insomnia (both initial and middle), decreased appetite with 12-pound weight loss, poor concentration, and passive suicidal ideation without plan or intent. Patient denies previous psychiatric treatment or hospitalizations. Patient reports increasing anxiety with worry about finances and health, accompanied by somatic symptoms including chest tightness, sweating, and shortness of breath occurring 3-4 times weekly.
COMPLETE MEDICAL HISTORY:
Hypertension diagnosed 3 years ago
Migraine headaches since age 25
Appendectomy at age 22
No history of head injuries, seizures, or loss of consciousness
No known drug allergies
CURRENT MEDICATIONS:
Lisinopril 10mg daily for hypertension
Sumatriptan 100mg PRN for migraines
Ibuprofen 400mg PRN for headaches
Melatonin 5mg nightly for sleep (self-prescribed, reports minimal benefit)
SUBSTANCE USE HISTORY:
Alcohol: 1-2 glasses of wine, 2-3 nights per week, increased to near-daily use in recent months
Tobacco: Denies
Cannabis: Occasional use (1-2 times monthly)
Other substances: Denies
FAMILY HISTORY:
Mother (age 65): History of depression, treated with medication
Father (age 67): Hypertension, Type 2 diabetes
Maternal grandmother: "Nervous breakdown" in her 40s, details unknown
Paternal grandfather: Alcoholism
MENTAL STATUS EXAMINATION ESTABLISHMENT:
- Appearance: Well-groomed female appearing stated age, appropriate casual attire
- Behavior: Cooperative, maintains appropriate eye contact, psychomotor retardation noted
- Speech: Soft in volume, normal rate, decreased spontaneity
- Mood: "Sad and worried"
- Affect: Constricted, congruent with reported mood
- Thought process: Linear and goal-directed
- Thought content: Preoccupation with health concerns and financial stressors, passive suicidal ideation without plan or intent, no homicidal ideation, no delusions
- Perception: No hallucinations or illusions
- Cognition: Alert and oriented x4, attention maintained throughout session, immediate and recent memory intact
- Insight: Good; acknowledges depression and anxiety affecting functioning
- Judgment: Intact; seeking appropriate treatment
PHYSICAL EXAM COMPONENT:
Vital Signs: BP 142/88, HR 88, RR 16, Temp 98.6°F
General: No acute distress, appears fatigued
HEENT: PERRL, EOMI, oropharynx clear
Neck: Supple, no thyromegaly
Cardiovascular: Regular rate and rhythm, no murmurs
Respiratory: Clear to auscultation bilaterally
Neurological: CN II-XII intact, no focal deficits, normal gait
RISK ASSESSMENT:
Suicide: Passive ideation without plan or intent; protective factors include desire for treatment, future-oriented goals
Homicide: No ideation, intent, or plan
Self-harm: No history or current ideation
Violence risk: Low; no history of aggression or violent behavior
MEDICAL NECESSITY:
Patient presents with significant symptoms of depression and anxiety causing marked impairment in social and occupational functioning. Comprehensive evaluation with medical assessment is necessary due to concurrent hypertension that may be exacerbated by anxiety, potential need for pharmacologic intervention, and to rule out medical contributors to presentation.
PSYCHIATRIC DIAGNOSIS:
F32.1 Major Depressive Disorder, single episode, moderate
F41.1 Generalized Anxiety Disorder
I10 Essential Hypertension
TREATMENT PLAN:
1. Start Sertraline 50mg daily for depression and anxiety, with planned titration to 100mg after 1 week if tolerated
2. Referral for individual psychotherapy services with focus on CBT for depression and anxiety
3. Recommend home blood pressure monitoring; patient to record readings twice daily
4. Continue current Lisinopril; will coordinate with PCP regarding management
5. Sleep hygiene education provided; recommended reduction of alcohol use
6. Follow-up appointment in 2 weeks to assess medication response and side effects
7. Provided crisis resources and safety planning
Patient verbalizes understanding of diagnosis, treatment options, medication side effects, and follow-up plan. Questions answered. Patient agrees with treatment plan.
Signature: ________________________ MD/DO/NP
Date/Time: 4/26/2025, 12:15 PM
Automating Therapy Notes with AI
Documentation is probably the least favorite activity of any mental health professional.
Did you know that now AI tools can write your Intake notes?
Technology has progressed such that there are now several AI products purpose-built for mental health professionals, that can listen in to your sessions and automatically generate robust, insurance-compliant Intake Notes. They can even write give suggestions for mental health assessment and possible mental health diagnosis.
Supanote is the leading AI Therapy Note tool - Supanote comes with prebuilt intake form templates and can accurately capture your intake session into an insurance-compliant note for billing with 90792. Curious? Here's a detailed guide to AI Therapy Note tools and how they work.
Ready to try? 10 notes on us!
Login to your Supanote account and instantly access 10 free notes
Get It Now!
Benefits of AI for 90792 Documentation
- Time-saving: AI can help generate structured documentation templates and suggest appropriate phrasing for clinical findings.
- Insurance-ready: Supanote for example is trained to write for insurance, so it will ensure all required elements for 90792 are included.
- Consistency: AI can help maintain consistent documentation standards across evaluations.
Important Considerations When Using AI
- Professional responsibility: The provider is always responsible for reviewing, editing, and ensuring the accuracy of all documentation, regardless of whether AI assistance was used.
- Medical components: Pay special attention to the medical aspects of the evaluation, as these distinguish 90792 from 90791 and must be accurately documented.
- Compliance: Verify that any AI tool used complies with HIPAA and other relevant regulations.
Common Mistakes to Avoid in Billing 90792
- Using 90792 when medical evaluation wasn't provided
- Insufficient documentation of physical exam component
- Billing 90792 by non-licensed physician providers
- Billing both diagnostic evaluation codes for the same day
- Missing add on codes when appropriate (like interactive complexity)
- Improper use of E M service codes in conjunction with 90792
Key Differences Between CPT code 90792 and 90791
Category | 90792 | 90791 |
|---|---|---|
Provider Eligibility | Only psychiatrists and other medical professionals | All mental health providers (e.g., therapists, social workers) |
Medical Components | Includes medical services (e.g., physical exam, medication evaluation) | No medical services included |
Reimbursement Rates | $185.18 (Medicare 2025) | $147–$160 (Medicare 2025 estimate) |
Documentation | Must document physical exam and medical assessment | No requirement for physical exam or medical assessment documentation |
Purpose | Comprehensive psychiatric evaluation with medical components | Psychiatric evaluation without medical components |
Comparing 90792 with Other Commonly Used Codes
90792 vs. E/M Codes (99202-99215)
Psychiatrists often need to decide between 90792 and E/M service codes:
- 90792: Used for comprehensive psychiatric diagnostic evaluations with medical components
- E/M Codes: Based on complexity of medical decision-making and/or time spent
Consider using E/M codes instead of 90792 for:
- Follow-up visits focusing primarily on medication management
- Shorter, less comprehensive visits
- When specific E/M code reimbursement rates are more favorable
90792 vs. Psychotherapy Codes
- 90832: 30-minute psychotherapy
- 90834: 45-minute psychotherapy
- 90837: 60-minute psychotherapy
These codes are often used in follow-up sessions after the initial 90792 evaluation.
90792 vs. Crisis Codes
- 90839/90840: Psychotherapy for crisis (first 60 minutes/each additional 30 minutes)
Note: You cannot bill 90792 and crisis codes on the same day for the same patient.
Tips for Clean Claims and Maximum Reimbursement
- Document thoroughly - Clearly note all medical services
- Verify benefits verification before the appointment
- Check if providers require pre-authorization - Many plans require this
- Submit claim form promptly - Implement daily claims filing
- Use electronic claim tracking when possible
- Include proper diagnosis codes that justify medical necessity
- Set up appointment reminders to reduce no-shows that affect billing
- Understand how treatment reported affects reimbursement
Frequently Asked Questions About CPT Code 90792
Q: Can I bill 90792 for telehealth services?
A: Yes, the psychiatric diagnostic evaluation with medical services can be billed for telehealth with the appropriate modifiers. Since the COVID-19 pandemic, most insurers have expanded coverage for behavioral health services via telehealth.
Q: How often can the same provider bill 90792 for the same client?
A: Most insurance companies allow one comprehensive evaluation per year. However, you may be able to bill another if there's a significant change in the patient's condition requiring a new psychiatric diagnostic assessment.
Q: What's the difference between using E/M service codes vs. 90792?
A: E/M service codes (99201-99215) are used primarily in medical settings and are based on complexity levels. The 90792 code is specific to psychiatric diagnostic evaluations with medical components and doesn't require meeting the same complexity criteria.
Q: Can clinical psychologists and clinical social worker professionals bill 90792?
A: No, these behavioral health providers cannot typically bill 90792 cpt code as they aren't authorized to provide the medical assessment components. They should use 90791 instead for diagnostic evaluation services.
Q: Can marriage and family therapists bill for diagnostic interviews?
A:Yes, marriage and family therapists can usually bill for diagnostic interviews using code 90791. They can’t use 90792 because that one involves medical services they’re not licensed to perform.
Q: What modifiers might apply when billing the 90792 cpt code?
A: Common modifiers include -25 (significant, separately identifiable E/M service), -95 or -GT (telehealth), -59 (distinct procedural service), and -52 (reduced services). Always check if providers require specific modifier usage for claim tracking purposes.
Q: How many times a year can you bill 90792 cpt code?
A: Most payers limit 90792 cpt code to once per calendar year per provider-patient relationship. However, this varies depending on the insurance carrier's specific policies. Medicare typically allows one 90792 per year unless medical necessity for an additional evaluation is clearly documented.
Conclusion
Mastering the 90792 CPT code isn't just about maximizing reimbursement—it's about accurately reflecting the comprehensive medical services you provide during a psychiatric evaluation to patients with mental disorders. By understanding the documentation requirements, implementing proper claim tracking, and avoiding common mistakes in billing, licensed mental health providers can reduce denied claims and focus more energy on providing quality behavioral health services.
Remember: The intake session depend heavily on proper documentation. When in doubt, document more rather than less. The time invested in proper documentation pays dividends in smoother insurance billing processes and fewer payment delays.
Resources for CPT Coding Support
- American Medical Association CPT® Code Resources
https://www.ama-assn.org/practice-management/cpt - Medicare Medicaid Services Mental Health Booklet
https://www.cms.gov/files/document/mln1986542-medicare-mental-health-coverage.pdf - American Psychiatric Association Coding Resources
https://www.apaservices.org/practice/reimbursement/health-codes - National Council for Behavioral Health Billing Guides
https://www.thenationalcouncil.org/resources/ - Top CPT Codes: Cheat Sheet and Examples
HIPAA-compliant AI Progress Notes for Psychologists and Mental Health Counselors. Save hours on Clinical Documentation.