Ever found yourself staring at a billing form, wondering if you're using the right code for that cognitive therapy session that ran longer than planned? You're not alone.
Many of us in clinical practice struggle with the nuances of current procedural terminology (CPT) coding, especially when it comes to cognitive function interventions.
The 97130 CPT code is particularly important for those of us providing cognitive function intervention services for patients with traumatic brain injury, dementia, and other disorders, and using it correctly can make a significant difference in both patient care and practice revenue.
What Exactly is the 97130 CPT Code?
According to the American Medical Association, CPT code 97130 is an "add-on code specifically designed for cognitive function intervention services that extend beyond the initial 15 minutes (which is billed under CPT code 97129)."
It represents each additional 15 minutes of one-on-one patient contact providing therapeutic interventions that focus on cognitive function, such as memory, executive function, and problem solving.
In coding guidelines, 97129 covers your first 15 minutes of cognitive therapy with a patient, and code 97130 covers each additional 15-minute block. This code must be listed separately in addition to the primary procedure. The structure allows for appropriate reimbursement and billing when therapy services require more time due to patient needs related to cognitive impairments.
When to Use CPT Code 97130
You should use CPT code 97130 when:
- You've already provided 15 minutes of cognitive function intervention (billed under 97129)
- You've delivered additional 15-minute increments of the same type of service
- The intervention involves direct one-on-one patient contact
- The therapy focuses on cognitive functions (attention, memory, reasoning, etc.)
- Services provided are considered medically necessary for the patient's condition
- The therapeutic interventions focus on helping patients manage the performance of an activity
Remember that 97130 cannot be used as a standalone code.
It must always be billed alongside the primary code 97129, which represents the initial 15 minutes of service. The focus should be on helping patients with compensatory strategies to manage time, sequencing tasks, and other cognitive skills affected by their medical conditions.
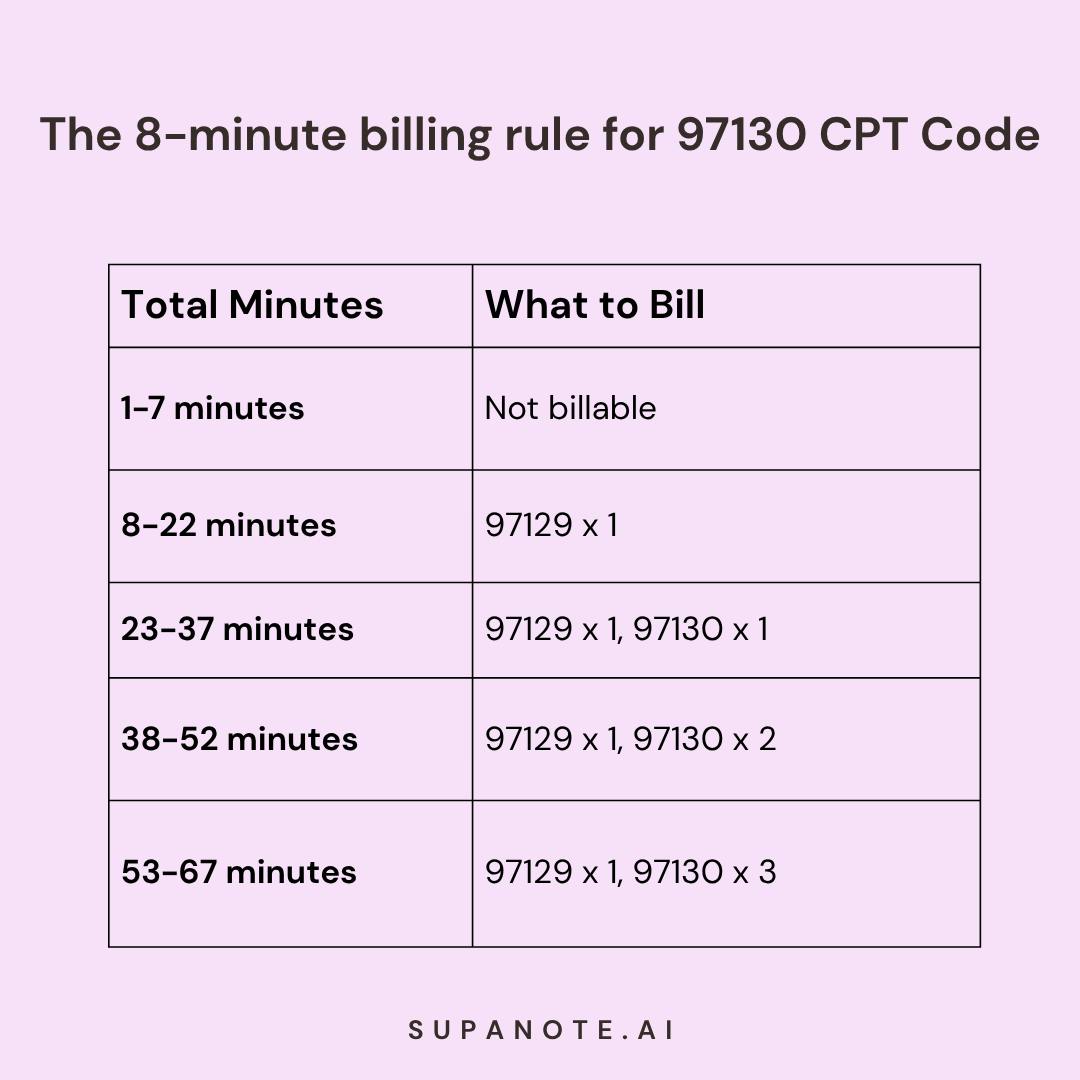
The 8-Minute Rule and Time Requirements
If you’ve billed any time-based therapy service before, you’re probably familiar with the 8-minute rule and 97130 follows the same math.
This rule helps determine how many units you can bill based on the additional time spent providing the service:
- To bill for the first unit (97129): At least 8 minutes of direct therapy
- To bill for a second unit (97130): At least 23 minutes total (full 15 minutes plus 8 additional minutes)
- For each additional unit: Complete the previous unit and exceed the halfway point of the next unit
The date of service should reflect when these therapeutic interventions were provided. For proper documentation and billing, track the exact time spent with each patient.
Here's a quick reference chart:
Documentation Requirements for 97130
Proper documentation is extremely crucial for reimbursement when using the 97130 CPT code.
Getting denied for missing one tiny detail? Been there too.
Here’s what to include to keep your 97130 claims airtight:
- Exact time tracking (start and end times for the session)
- Specific cognitive interventions provided
- Medical necessity linking the treatment to the patient's condition
- Patient's response to the interventions
- Progress toward treatment goals
- Plans for future sessions
Your notes should demonstrate how the therapeutic interventions address the patient's cognitive impairments and how these interventions help the patient manage the performance of an activity. Documentation should support why additional time beyond the initial 15 minutes was necessary.
For example, your notes might include:
"45-minute cognitive therapy session (2:00-2:45 PM). First 15 minutes focused on attention training exercises, followed by 30 minutes of executive function activities using problem-solving tasks. Patient demonstrated improved ability to maintain focus for up to 10 minutes compared to 5 minutes in previous session. Compensatory strategies for managing time and sequencing tasks were introduced to address difficulties with daily activities."
Note-Taking Made Easy for Therapists
Accurate, time-saving documentation that’s built for your billing codes
Try Supanote for Free Now!
Common Diagnoses for 97130 Billing
The 97130 CPT code is typically used for patients with conditions that affect cognitive function, such as:
- Traumatic brain injury (TBI)
- Cerebral infarction
- Nontraumatic intracerebral hemorrhage and other nontraumatic intracranial hemorrhage
- Neurodegenerative diseases (Alzheimer's, Parkinson's)
- Dementia
- Brain cancer
- Learning disabilities
- Developmental disorders affecting psychological development
- Communication disorders
- Post-concussion syndrome
- Cognitive symptoms related to mental health conditions
Always ensure your diagnosis code (ICD-10) appropriately matches the cognitive function intervention services you're providing to avoid claim denials. Medical necessity must be well-documented for neurological conditions requiring these specialized therapeutic interventions.
Insurance Coverage and Reimbursement
Coverage and reimbursement for 97130 varies by insurer:
- Medicare typically covers 97130 when deemed medically necessary for treatment of cognitive impairments
- Private insurance policies may have specific requirements, fee schedules, or limitations
- Medicaid coverage is state-dependent
Always verify coverage before providing extended cognitive function intervention services. Payer policies can differ significantly regarding these therapeutic interventions. Many insurers require prior authorization for cognitive therapy services, especially in skilled nursing facilities or for extended treatment plans.
Understanding different fee schedules and reimbursement rates for these services can help optimize your practice's financial performance while providing necessary care. Treatment guidelines from professional organizations can help establish medical necessity for these services.
Common Billing Mistakes to Avoid
When billing with the 97130 CPT code, avoid these common pitfalls:
- Using 97130 without 97129 - Remember, 97130 is an add-on code and cannot be reported alone
- Inaccurate time tracking - Document your session times precisely to justify additional time
- Insufficient medical necessity documentation - Clearly establish why extended cognitive function intervention is needed
- Not using required modifiers - Some insurers require specific modifiers (like GP for physical therapy, GO for occupational therapy, etc.)
- Billing for non-direct services - Only one-on-one patient contact counts toward 97130
- Failing to verify coverage - Always check payer policies before providing extended services
- Missing documentation of performance improvement - Show how therapy helps patients manage and perform activities
Have your progress notes written for you automatically
Cognitive therapy notes—done in seconds
Try it Out for Free!
Interdisciplinary Considerations
While psychologists commonly use the 97129/97130 codes, they're also used by other professionals providing therapy services:
- Occupational therapists
- Speech language pathology professionals
- Physical therapists
- Physicians
- Other qualified healthcare professionals treating cognitive impairments
Speech language pathologists frequently use these codes when addressing cognitive aspects of communication disorders. The focus on cognitive function makes these codes applicable across multiple disciplines that treat neurological and developmental disorders.
This interdisciplinary usage can sometimes create confusion in treatment settings. When working in a team, it's important to coordinate on who will be billing for cognitive function intervention services to avoid duplicate billing for the same treatment time. Different documentation requirements may apply depending on the provider type and practice setting, including skilled nursing facilities.
Automating Therapy Notes with AI
Documenting cognitive therapy , especially for add-on codes like 97130 an eat into your clinical time fast. That’s why many providers now use AI Therapy Note tools like Supanote to streamline the process.
Supanote helps automate detailed progress notes for extended cognitive function sessions, capturing what really matters: how time was spent, which interventions you used, and how your patient actually responded in the moment.
It recognizes therapy length, structures notes using templates like SOAP, DAP, GIRP, BIRP and ensures every session meets payer requirements for time-based billing codes. With prebuilt, easy-to-use templates, writing thorough notes becomes faster, more accurate, and less stressful.
Here's a detailed guide to AI Therapy Note tools and how they work.
Frequently Asked Questions About 97130 CPT Code
Q: Can 97130 be used for telehealth sessions?
A: Yes, many insurers allow the 97130 CPT code for telehealth cognitive therapy. Use the appropriate telehealth modifier (typically 95) and verify coverage with the specific insurer before services are provided.
Q: How many units of 97130 can I bill in one day?
A: Medicare's Medically Unlikely Edit (MUE) allows up to 5 units of 97130 per day, but medical necessity must be documented for extended sessions focusing on cognitive function and performance.
Q: Can I bill 97130 alongside other therapy codes on the same day?
A: It depends on the payer policies. Some insurers may not allow 97130 to be billed with other therapy services (like 90834) on the same day. Always check payer-specific guidelines regarding cognitive function intervention services.
Q: Do I need special certification to bill 97130?
A: While no specific certification is required, you must be qualified to provide cognitive therapy services within your scope of practice. Documentation should support your ability to deliver these therapeutic interventions.
Q: How does 97130 differ from psychotherapy codes like 90834?
A: 97130 is specifically for cognitive rehabilitation interventions (memory, executive function, etc.), while 90834 is for psychotherapy addressing emotional and behavioral issues. They represent different types of treatment with different goals for patient care.
Q: Can group cognitive therapy be billed using 97130?
A: No, 97130 is specifically for one-on-one patient contact. Group therapy should be billed using appropriate group therapy codes, as these codes require direct intervention with a single patient to manage the performance of activities.
Q: What modifiers might be needed with 97130?
A: Depending on the provider type and setting, you might need modifiers like:
- GP (physical therapy)
- GO (occupational therapy)
- GN (speech language pathology)
- 95 (telehealth)
Q: Is prior authorization typically required for 97130?
A: Many insurers require prior authorization for cognitive function intervention services, especially for patients with neurodegenerative diseases, traumatic brain injury, or other neurological conditions. Always verify coverage requirements before treatment.
Conclusion
Understanding and using the 97130 CPT code correctly isn’t just about clean billing, it’s about accurately reflecting the time and care you invest in helping patients work through serious cognitive challenges.
Whether you’re supporting someone with traumatic brain injury, cerebral infarction, dementia, or a learning disorder, these interventions aren’t optional—they’re life-changing. You're helping patients rebuild skills like memory, task sequencing, and problem-solving so they can regain independence and confidence in their daily routines.
That’s why tracking session time precisely, documenting thoroughly, and staying current with payer guidelines matters so much. When your notes are strong, your billing is solid—and you get more time back to focus on what really counts: your patient’s progress.
And remember, billing rules and coding guidance don’t stay static. It’s worth checking in now and then with updates from the AMA, Medicare, or individual insurers to make sure your billing practices stay compliant and your claims don’t get held up.
Want help streamlining your 97130 documentation and reducing billing errors?
Try Supanote for Free Now!

