You need therapy notes that work. Not lengthy documentation that eats into your lunch break or evening family time.
Good news: The right template cuts your documentation time in half. Even better news: Supanote takes your session and delivers a complete, HIPAA-compliant note automatically.
This guide gives you the exact templates that work in real practice. You'll get actual examples you can adapt today, plus tips that veteran therapists wish they'd known years ago.
Therapy Notes Template Overview
The therapy notes template is a structured format that aids clinicians in documenting details about each session..
A standard template often has the following elements:
- Client Details: Name, contact information, dates of sessions, and other relevant identifiers.
- Session Information: Time and duration of the session, session type (telehealth or in-person), and any relevant clinical settings.
- Observations: Verbal and nonverbal cues observed during the session.
- Interventions: Specific techniques or approaches used during the session.
- Progress Notes: An account of how therapy is unfolding over time, including objective measures and subjective reports.
- Plans: Future goals, homework assignments, or strategies for upcoming sessions.
A well-crafted therapy notes template also meets privacy standards, such as HIPAA compliance, ensuring that sensitive client data remains secure.
Top 3 Therapy Note Templates for Clinicians
Among the most widely used are SOAP, DAP, and BIRP. Each comes with its own set of benefits and serves specific purposes during clinical documentation.
- Subjective: Captures the client’s expressed feelings, symptoms, and concerns.
- Objective: Involves the clinician’s observations, such as body language, tone of voice, and other measurable data.
- Assessment: Provides interpretation based on the subjective and objective information, including any potential diagnoses.
- Plan: Outlines steps for future sessions, such as interventions, goals, or exercises.
DAP Format:
- Description: Offers a narrative account of the events during the session.
- Assessment: Reflects the clinician’s interpretation of the session, including insights into the client’s progress.
- Plan: Details the next steps, often incorporating both therapeutic interventions and client homework.
BIRP Format:
- Behavior: Focuses on observable client behavior during the session.
- Intervention: Lists the techniques and strategies the clinician used during the discussion.
- Response: Describes how the client reacted to the interventions.
- Plan: Sketches out future plans, such as follow-up strategies or additional interventions.
Best Therapy Notes Templates for Efficient Documentation
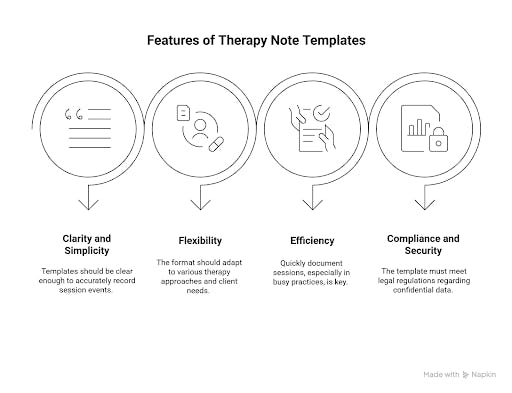
Choosing among the many available formats often causes questions about the best therapy notes templates. The best formats usually share certain features:
- Templates should be clear enough to record session events accurately without getting bogged down in lengthy descriptions.
- The format should adapt to various therapy approaches.
- Being able to quickly document sessions is key, especially in busy practices.
- Digital note-taking platforms often come with features that adhere to HIPAA, PHIPA, or GDPR standards and offer enhanced security through encryption.
Therapy Notes Examples Using SOAP, DAP, and BIRP Formats
Clear therapy notes examples can provide a reference point for those new to structured documentation. Below are examples using three commonly adopted formats.
SOAP Example - Anxiety Case
S: "I had three panic attacks this week. The breathing technique helped once."
O: Client demonstrated proper breathing technique. Hands are trembling slightly.
A: Panic disorder with improvement. The client is implementing coping skills independently.
P: Continue exposure work. Add progressive muscle relaxation. Consider a psychiatry referral if no improvement in 2 weeks.
DAP Example - Couples Session
D: Couples argued about finances for 20 minutes. Partner A raised their voice twice. Partner B shut down, arms crossed. I intervened with the timeout technique.
A: Communication patterns remain defensive. Both were triggered by money discussions stemming from childhood experiences.
P: Assign speaker-listener exercise for home. Focus next session on childhood money messages.
BIRP Example - Teen Depression
B: The Teen looked at the phone 6 times during the session. Smiled when discussing weekend plans with friends.
I: Set the phone boundary. Explored social connections as a protective factor. Assigned mood tracking app.
R: Agreed to phone boundary after initial protest. Engaged when discussing friends. Downloaded the app in session.
P: Review mood data next week. Build on social strengths. Parent check-in regarding screen time..
Enhance Your Therapy Notes Template Process with Supanote
Supanote AI offers a platform that transforms session audio into well-organized therapy notes. The tool is designed with input from clinicians to meet the high demands of clinical practice.
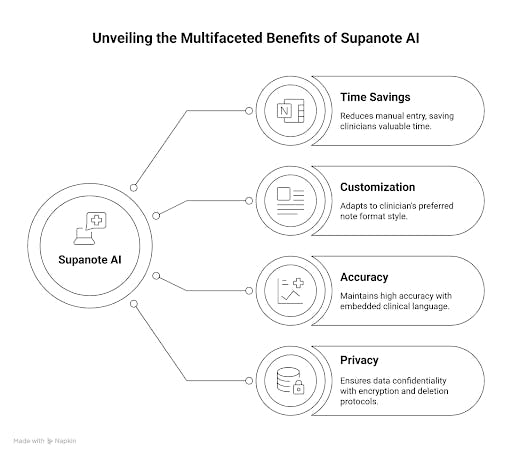
Key advantages include:
- Time Savings: Automatically generating notes from dictated sessions helps reduce the burden of manual entry.
- Customization: Enhancements allow the note format to match the clinician’s preferred style. Whether using SOAP, DAP, or BIRP, the platform adapts to the template that works best for the practitioner.
- Accuracy: With clinical language embedded in the system, the generated notes maintain a high level of accuracy indispensable for ongoing care and treatment decisions.
- Privacy: Built with full encryption and automatic deletion protocols, the tool ensures that sensitive data remains confidential.
Therapy Notes Template Tips for Accurate Documentation
Consistency in documentation is essential for maintaining reliable client records. Here are some practical tips to improve your note-taking process:
- Choose a template, whether SOAP, DAP, BIRP, or a custom design that suits your practice.
- Use straightforward language to describe sessions. Avoid overly lengthy details that may cloud the main points of the session.
- Objective details can sometimes highlight issues that the client may not be fully aware of.
- Timely documentation ensures that details remain fresh and important observations are not forgotten.
- Always use a secure digital platform that meets privacy standards.
- Verifying the content after each session can help catch minor errors and improve overall clarity before the record becomes part of the official file.
Conclusion
Your therapy notes serve three masters: clinical care, legal protection, and insurance requirements. The right template satisfies all three without eating your life.
Start with SOAP if you're unsure. It works everywhere. Use consistent formatting. Time yourself - 10 minutes maximum per note.
Consider digital tools when your hand cramps from writing or you're staying late to finish notes. Supanote AI and similar platforms give you time back for what matters: helping clients.
Your clients need your clinical skills, not your novel-writing abilities. Keep notes clear, complete, and concise. That's the formula that works.
FAQs
Q1. What is a therapy notes template?
A therapy notes template is a structured format that helps clinicians record client session details clearly. It includes sections for observations, interventions, and future plans, ensuring accurate record-keeping.
Q2. What are the top therapy note templates used by mental health professionals?
The most common templates include SOAP (Subjective, Objective, Assessment, Plan), DAP (Description, Assessment, Plan), and BIRP (Behavior, Intervention, Response, Plan). These formats are preferred for their clarity and ease of use.
Q3. How do therapy notes templates improve clinical documentation?
They standardize the documentation process, making it easier to capture and review session details. A consistent format helps maintain accuracy and supports better treatment planning.
Q4. How can digital tools like Supanote AI help in creating therapy notes?
Digital tools can quickly convert session audio into structured notes, reducing the manual workload for clinicians. They ensure high accuracy and adherence to data privacy standards while saving valuable time.
Q5. What factors should I consider when choosing a therapy notes template?
Consider the template’s clarity, flexibility, and compliance with privacy regulations. Choose a format that aligns with your clinical style and meets the specific documentation needs of your practice.
Q6: What's the biggest documentation mistake new therapists make?
Writing notes like academic papers. Your note isn't a dissertation. It's a practical tool for continuity of care.
Q7: How do I document when a client refuses an intervention?
Note the refusal, their stated reason, and your alternative plan. "Client declined medication referral, citing preference for therapy alone. Will reassess in 4 weeks."
Q8: Should I document my clinical hunches?
Yes, but label them clearly. "Clinical impression: possible trauma history based on avoidance patterns. Will explore gently in future sessions."
Q9: How often should I mention treatment goals in notes?
Every 3-4 sessions minimum. Show progress toward goals or explain why you're adjusting them.